Prostate cancer and its treatment can be a life and life-style changing experience for any man. This blog tracks one gay man’s 5 year experience (January 2016 to July 2021) and has been written to provide some context for other men who may be faced with the same diagnosis.
Attention to the Reader: The following text, images and links provide the reader with a detailed week-by-week adventure, before and after the blogger’s diagnosis of prostate cancer. This blog’s site was created to provide both gay and straight men, who have been given a diagnosis of prostate cancer, a better understanding of what to expect as they work through their decision on treatment options. Sometimes the images are graphic, occasionally the wording is very descriptive of an experience or situation. The site hopes to inform and educate the reader through the experiences of the blogger.
About the Blogger: CityGuyTX is a screen name of a now 71 year old, single gay man living in Houston, Texas. The blogger’s professional background is in the area of medical devices, their marketing and sales. With the onset of the COVID Pandemic of 2020, the blogger decided to retire from a consultant position that involved marketing and sales development of a nerve monitoring accessory for the the DaVinci Systems surgical robot – as it is configured to be used in robotic prostatectomies. The blogger now has time to enjoy full time two hobbies – MIDI keyboard music and high-end camera videography.
The Cast of Characters: To provide some anonymity to my physicians and their staff I’ve elected to label my physicians by the order in which they appear in the blog. Dr. A – a specialist in oncology; Dr. B – a urologic oncologist and highly trained da Vinci robotic surgeon; Dr. C – a radiology oncologist whose specialty area is Cyberknife, stereotaxic body radiation therapy (SBRT).
Prologue: In the late 80s I moved to Houston from Dallas because of the growing importance of the Texas Medical Center in my professional career. The move proved to be a good one and I soon became one of my company’s leading sales and marketing persons. The move to Houston, being in a completely new city where few people knew me – presented me with an ideal situation to explore homosexual interests which I’d long submerged in my work. The late 1980s was also a time when the HIV epidemic was just beginning to impact the Houston’s gay community. It was during this time that I met the physician who would become my personal internist – although his clinical specialty was oncology. Dr. A was active in treatment of AIDs patients because of the frequent appearance of Karposi Sarcoma that developed because of a suppressed immune system. One afternoon at the funeral of an acquaintance who had died of AIDs I asked Dr. A if he would accept me as a patient – he said yes, and thus began a 25 year patient / physician relationship.
The PSA test became a standard part of the blood work for my annual physical with Dr. A. As I got older the PSA values began to increase 2001 – 2.8 ng/ml; 2009 – 3.1 ng/ml; 2011 – 4.4 ng/ml; 2013 – 6.4 ng/ml. Dr. A didn’t voice a heightened concern with the PSA being over the long cited, upper “normal range” value of 4.0 ng/ml as my digital rectal examination (DRE) indicated an enlarged prostate. Benign prostate hyperplasia (BPH -prostate enlargement) also impacts the PSA score. The larger the prostate, the higher the PSA score.
The PSA test for my physical in mid-December 2015 came back as 7.0 ng/ml and Free-PSA as 10.6. These values equated to about a 35% chance that there was some level of cancerous lesion in the prostate. Dr. A suggested that I repeat the PSA test, as the test’s score can be impacted by a number of factors: undefined prostatitis and/or sexual activity (masturbation with ejaculation, anal intercourse) within a 3-5 day period to the blood sample being drawn may cause an elevated PSA level.
The second test, drawn at during the last week in December came back even higher – a PSA of 9.7 ng/ml and a Free PSA of 17.9 ng/ml. These values equate to about a 23% chance that there was come level of cancerous lesion in the prostate – a statistical chance lower than the earlier mid-December 2015 test. However, Dr. A suggested that he schedule an appointment with a urologic oncologist specialist in the Texas Medical Center. He felt that I would like Dr. B, who was an internationally known specialist in prostate cancer.
January 2016:
Week of 1/03 – Not having received any confirmation from Dr. A’s office that he had made a referral appointment for me with Dr. B, I called and talked with Dr. A’s nurse on 1/07. She indicated she would remind Dr. A – as he had been out of town the first part of the week.
Week of 1/10 – Still not receiving a call from Dr. A’s office by the afternoon of 1/14, I decided to go to Dr. B’s office and make an appointment the next day. Registering as a new patient of Dr. B was a breeze (surprise) and an appointment was made to see him on February 2nd at 11:15 AM (his first clinic patient of the day). During the registration a tall lady appears and looked over the shoulder of the lady doing the registration. She came back shortly and introduced herself as the urology group’s clinic nurse manager. I briefly told her I’d been referred to Dr. B by Dr. A. She said she had known Dr. A for years and immediately pulled out her cell phone and called him. Dr. A picked up on her call and she told him that I’d just registered as a patient. While I couldn’t hear all of their conversation – it was obvious that she and he had an excellent professional relationship which went back a long time. At the end of their cell phone conversation, the clinic nurse manager indicated she would request my records from Dr. A and looked forward to working with me as a patient of Dr. B. She gave me her calling card and indicated that if I had any questions, I could call or e-mail her.
Week of 1/17 – No activity
Week of 1/24 – Arranged to repeat the blood work of late December. Blood was drawn at LabCorp – Houston, on 1/28. I had arranged for the results to be sent via e-mail PDF file, so that the most recent blood chemistry would be available for my initial meeting with Dr. B on 2/02 The Total PSA value had dropped from 9.7 to 4.9 ng/ml.
February 2016
Week of 1/31 – The scheduled initial meeting on with Dr. B on 2/2 got delayed by an hour – arriving he apologized, saying his staff had over-booked him that morning. In reviewing his background, I had been a bit concerned about Dr. B’s age. However, that concern was immediately dissuaded with his firm handshake, smile and tinkle in the eyes. Dr. A was correct – Dr. B was immediately likable. We spent about 20 minutes discussing some of my health history. I indicated to him that I’d like to have a PCA3 test run to help sort out the possibility of prostate cancer. He indicated that he generally does that on an initial visit, as well as ordering a pelvic/prostate MRI.
The PCA3 test relies upon analysis of cellular mRNA (messenger ribonucleic acid) from cells excreted in the seminal fluid, via urine flow, after a prostate massage. This gene test can further validate the presence of prostate cancer, as the gene expression of the PCA3 antigen is 60-100 times greater in cancerous tissue than in benign prostate tissue. The PCA3 test value is not impacted by the size of the prostate. See: (http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2556484/ ) for more details.
Dr. B indicated that he’d now like to collect a sample for the PCA3 test. He raised the examination table to about pelvic height and asked me to drop my pants, underwear and lean forward over the examination table – basically the same position as it frequently used for a digital rectal examination (DRE). He proceeded with his gloved hand to perform a DRE. He indicated that my prostate surface was smooth with no surface bumps or irregularities – which was a good sign. (Irregularities of the surface suggest tumor growth outside the prostate). He then indicated that he was going to make some very forceful finger pressures on the prostate. This consisted of four (4) forceful compressions of the right and left lobes of the organ. There was a bit of discomfort but no pain associated with the experience. He opened a drawer in the examination room desk and pulled out a urinalysis collection cup. He gave me a box of tissue to clean up the lubricant from my rectal area and said there was a rest room across the hall and I could void the urine sample there. Returning to the examination room, Dr. B’s clinic nurse manager was there with some forms for the MRI examine. I gave her the urine sample. She indicated that it would probably be 10 days before they would have the results of the PCA3 test. In the intervening time I should have a MRI scan.
The initial first visit impressions of the urologist’s office had been tempered by Dr. B and his clinic nurse manager. This was a physician and clinic nurse in whom I could put confidence. The decisions I’d be making over the next couple of week would impact the rest of my life as a gay man.
In leaving the office I was struck by the number of men accompanied by their wives filling the waiting area. One could see the concern, uncertainty in their faces. Interestingly the vast majority of the men looked older than me – although many were probably my age or younger. I recalled a passing comment made by a gay friend – he indicated that he felt that married men aged faster than gay men! That’s only one gay man’s thoughts – prostate cancer certainly doesn’t discriminate between sexual preferences!
Later that same day, I received a phone call from the MRI center. The MRI was scheduled for 2/09. The staff person making the schedule indicated I should take a fleet enema the morning of the MRI and should abstain from any sexual activity 4 days prior to the MRI. The last request was a bit interesting. A Google search revealed the answer – recent ejaculation can influence the quality of the MRI image and make interpretation of the prostate’s image more difficult.
It’s amazing what information one can find on the Internet and on one site – YouTube – in particular. Thursday afternoon (2/04) I discovered a number of videos showing actual da Vinci robotic prostatectomies. A very completed video from The Urology and Prostate Institute of San Antonio, see ( https://www.youtube.com/watch?v=ZchNF25kALw ), caught my attention, as it utilized a nerve conduction monitor from a medical device company located in Austin TX . The monitor allows the surgeon, during the surgery, to assess the location of the parasympathetic nerve bundle (responsible for the penis filling with blood and becoming semi-erect) and the somatic /perineal nerves that are responsible for muscular action which then blocks the venous outflow from the penis (resulting in a fully hard erection). The parasympathetic nerve bundle is fairly easily visualized in surgery, however the somatic /perineal nerves are invisible to the eye (even with robotic surgery and the enhanced visual magnification of the visual field). The company’s instrumentation detects the presence of these invisible somatic / perineal nerves during the surgical dissection. This is accomplished by stimulating surrounding tissue with a low-voltage pulse. If there are critical nerves within the stimulated tissue, an “action potential” is generated and will be seen in the da Vinci console monitor screen and a “twitch will be seen in the pelvic musculature by the surgeon on the console monitor. I thought WOW, this really adds a high level of assurance that the nerves responsible for bladder control and the penal erection will not be inadvertently damaged during the surgical procedure. A visit to the company’s website provided more information about the nerve monitor, as well as a listing urologists in various states who utilized their instrument during prostatectomies. There were surgeons listed in Dallas, Austin, San Antonio, El Paso and Texarkana – BUT NONE IN HOUSTON ! Was this simply because their website page needed to be updated or were there no urological surgeons in the 4th largest city in the USA using the nerve monitor?
Friday morning (2/5) at 9:35 AM I called the medical device company’s office in Austin, Texas and left a message and call back # on the company’s “For All Other Inquires” phone option. Fifteen minutes later I received a phone call from one of the company founders, who also served as VP of Sales and Marketing. He indicated that there was no urologic surgeon in Houston currently using their instrument. He indicated that the cost of the system, per patient surgery, was about $ 1,000.00 and that hospitals generally feel they are already losing money on robotic surgery of the prostate. He felt it was a difficult sell to have them tack on another $ 1,000.00 to the $ 9,000.00 per patient cost of the surgery when the da Vinci robotic system was used. I asked him what if the patient – me – paid that $ 1,000.00? A bit surprised at my offer, he said that even under that scenario, using it would require approval from the hospital’s administration and would be very time consuming. Our conversation lasted about an hour. My background in medical device sales proved to be quite useful in the conversation. I asked him, as they have no users in Houston, if I could convince Dr. B to incorporate their nerve monitor into a prostatectomy that I might undergo, would the company provide staffing support in the OR for Dr. B to make sure the instrumentation was utilized during my surgery correctly. The VP of Sales and Marketing indicated certainly that would be the case – in fact, he said he would personally head up their team.
As the company’s nerve monitor seemed to be such a PLUS for this type of surgery – I began to consider my options if the MRI scan or PCA3 test came back positive for cancer. What I now knew about nerve sparing during the da Vinci robotic prostatectomy, if Dr. B declined my offer of a “free to the hospital” nerve monitor evaluation during an actual prostatectomy (mine) – I would have to consider other urologists outside Houston, who used the company’s instrument in their robotic prostatectomies.
Week of 2/07 – Tuesday morning, 2/9, after a fleet enema, I arrived at the MRI facility around 10:15 AM. After not too long a wait, a MRI technician directed me to a dressing room indicating I needed to change down to a dressing gown before the procedure. He indicated that they would be using an image enhancement dye – gadolinium – as part of the procedure. He took great care in finding a vein in my left arm and inserted a needle cannula and taped in down securely. He indicated that the dye injection would be at the end of the 30-40 minute scan series. He helped me lay down on the MRI gurney and strapped two different harnesses over the lower portion of my torso and pulled them tight to minimize body movement during the scans. He gave me some headphone to dampen the noise of the device, positioned my left cannulated arm over my chest and gave me a “panic button” bulb for my right hand. Shortly after him leaving the room, the gurney began to move forward and the initial scans began. The scans lasted about 30 minutes. About 15 minutes into all this my lower back began to pain me; I thought I should have asked for another pillow to use as a lumbar support. Too late now. After about 20 minutes of scans, he entered the room and began to prepare the gadolinium injection. I asked him for a pillow and putting that under my back as added support eliminated the pain discomfort. The gadolinium injection complete, he returned to the MRI controls and the final scan began. This took about 10 minutes. The MRI scan completed he removed the body restraints, helped me to a sitting position on the gurney and removed the cannula from my left arm and put a pressure dressing on the area. He wanted to know if I wanted a CDROM of the scan images – Yes I did. He also indicated that the images would be available online at the MRI Center’s website later in the afternoon and could be viewed via a username and password which would be given me when I checked out. I went back to the dressing room, got dressed and then went to the check-out desk. Telling the staff the desk I wanted a CDROM of the image they said it would take about 5 minutes to make it. The staff indicated that it would be 2 to 3 days before the radiologist report would be forwarded to Dr. B.
On Thursday, 2/11, the clinic nurse manager called me – she indicated that the MRI results came back as “normal” with no indication of loci of malignancy. However, the PCA3 test value was 120 – where 25-30 is generally considered a normal cut-off number. So the PCA3 was positive for malignant cells in the prostate fluid BUT the MRI dye enhancement technique for prostate cancer showed negative. The nurse manager indicated that Dr. B would like to schedule me for a prostate biopsy on 4/21 to help clarify the PCA3 and MRI results. I asked her why the 60 day delay – she indicated that was the first available slot in his schedule. She indicated I would need to take antibiotics prior to the biopsy and would send me via e-mail instructions later in the week.
A 60 day delay after the PCA3 showed positive for malignant cells seemed to me to be a bit unusual. My personal take on this was that Dr. B was placing more confidence in the MRI scan than in the new genomic PCA3 test.
On Saturday, 2/13, my SKYPE friend in Washington DC sent me one of his usual “Morning” from his iPhone. Tom is a civil engineer with a construction company that does work all over the USA. In an earlier conversation with Tom I learned that 6 years ago his older partner had experienced a rise in his PSA levels – from 3.0 ng/ml to 5.5 ng/ml – over a 12 month period. His partner had elected to use a relatively new type of radiation therapy – Cyberknife.
Having not taken time to research the Cyberknife technology, I asked Tom more about his partner’s experience with Cyberknife. He said that the worse part for his partner was placement of the gold fiducials (marker pellets) into the prostate, so that the Cyberknife can track prostate location and body movement during the treatments. The radiation treatment were easy and his partner was back to work in the week following the therapy. However, he did experience a reduction in energy level (associated with the radiation therapy). There was also a period of about 6 weeks where there was blood mixed with the urine as well as with ejaculate fluid. As the MRI dye scans showed multiple loci of malignancy in his partner’s prostate, they didn’t do a biopsy prior to beginning Cyberknife. Tom indicated that his partner has had no problems with urinary incontinence and no problem with erections – however, the amount of semen now ejaculated is small and sometimes none. However, his neural connections to have a physical climax are still intact. Tom indicated that initially there was a problem with his partner’s insurance provider covering the cost of the Cyberknife, but eventually that was resolved and he had the treatment sessions done at a hospital in Arlington, about a 10 minute drive from where they lived.
Week of 2/14 – On Monday, 2/15 I receive an survey from Dr. B’s hospital regarding my visit with Dr. B. It was a simple “check the box” questionnaire. However, at the end was a space for additional comments. In that space I typed:
In the post-visit research I conducted on robotic prostatectomy, I was surprised to learn that the hospital’s Urology Group did not have access / utilized a real-time nerve monitoring system provided by a medical device company in Austin TX. The system is specifically designed to be used with the da Vinci robotic instrument. Urology surgeons in Dallas, Fort Worth, Austin, San Antonio and even Texarkana use the company’s system to reduce the possibility of inadvertent nerve injury during the surgical procedure. In talking with the management of the Austin-based company – it would seem that no urology surgeon in Houston uses this system. The lack of the use of the company’s system in the hospital’s Urology Department has made me assess having surgery (if recommended) by any physician associated with the department.
I copied my comments in the survey to the medical device company’s VP of Marketing and Sales in a short e-mail. On 2/16 I received a reply back from him.
Thanks for pushing the technology. I am traveling this week and next but we need to get together ASAP and discuss the details and get you trained so we can get you started. It would be good if we can get you into a live surgery, most likely here in Austin. I will get back to you with some dates as soon as possible.
Interesting reply from the company’s management – they would seem to be genuinely interested in me become associated with them to represent their instrument – at least here in the Houston area.
Week of 2/21 – Friday, 2/26, have blood drawn at LabCorp for another PSA test. The phlebotomist commented that his father has a high PSA value and that he should really have a test done himself as a baseline – even though he was in his mid-30s.
March 2016
Week of 2/28 – Monday 2/29, it’s a LEAP YEAR ! Tuesday, 3/1, the results come back from LabCorp – PSA = 5.7 – so up 0.8 points from the last test on 1/28 – which was 4.9. A bit of a disappointment, but not overly concerned because of the seeming erratic values which the test provides – at least for me. Still would been nice to see the value decrease 0.8 rather than increase. The afternoon of 3/2, I called the Cyberknife facility and left a message on their phone recorder. A lady called back in about 1 hours and asked questions about insurance and referrals from the other physicians I’m seeing. She indicates that a Dr.C is accepting new patients for prostate treatment with the Cyberknife. I indicate that because of some prior commitments for a meeting in Austin the week of 3/06, I wasn’t sure when that week I’d be in the Houston area – and could meet with Dr. C. She indicated she too would need to check his schedule and indicated that when I knew my schedule to call back and she would set something up.
About 5:30PM on 3/02, Dr. C called me on my cell phone. We talked about 45 minutes as I gave him some background on how I’d come to consider the Cyberknife option. His call was quite unexpected on my part – I’d not had time to do some research on his background. He was surprised that Dr. B (nor any other urologist in Houston) was not using the nerve monitoring instrument. He indicated he would send me PDF files of some recently published clinicals on the use of the Cyberknife. I told him I was in the process later that evening in putting together info on my PSA tests and faxing them to his office. I told him I would send him a link to my MRI scans. About 30 minutes after the conversation an e-mail containing the PDF files were received from Dr. C. Later that evening I faxed a 5 page document to his office with sheets from the 4 LabCorp PSA tests.
On Friday, 3/04, as I’d not received any correspondence from the nerve monitoring company giving me a meeting date in Austin, I called scheduler at the Cyberknife facility. The scheduler indicated she had never received the fax, and gave me another number to send it. She too indicated that while she could schedule a meeting with Dr. C, he had told her that he would prefer that he too have information from the biopsy, prior to making any decision about my suitability for Cyberknife treatment. I told her that I would like to meet with him briefly before the 4/21 biopsy date. She indicated that could be arranged. Faxes were again sent and received at the other phone #.
Week of 3/08 – Monday, 3/7, at 9:15 AM receive a phone call from the VP of Marketing and Sales – suggesting that I meet with them on Friday, 3/11, in Austin. He indicates he will arrange for hotel accommodations at a Sonesta Hotel, not too far distance from their Austin office. He asked about how I was doing with my “condition”. I indicated that since we last talked I’d met with the director of the Cyberknife facility here in Houston. Because it would require me to go to either Austin or San Antonio to have surgery where the nerve monitor is being used in prostatectomy and as I have no personal “support system” in either of those cities – I’d pretty much decided (pending biopsy findings) to select the Cyberknife. He said that with radiology therapy there is a higher potential for reoccurrence of prostate-related cancer over time (obviously, one is not removing the prostate). But like the urologist who does surgery, the VP’s remarks were also colored by the fact that his company has a product that is used in that surgery. One of the issues that men face in prostate cancer is the “bias” in what they hear about treatment options, when talking with their physician or urologist. The complexity of treatment options is made even more difficult by the fact that every man’s cancer profile will be different.
Week of 3/13 – No activity
Week of 3/20 – No activity
Week of 3/27 – No activity
April 2016
Week of 4/04 – No activity
Week of 4/10 – After the biopsy planned for the 21st, the PSA values will be screwed up for a least 6 months – so felt it was important to have a PSA drawn late this week to see what had changed since the early March PSA . I again ordered a blood test from Life Extension. As PSA doesn’t require fasting, I had the blood drawn the afternoon of 4/14 – one week from the biopsy date. The results arrived on Saturday, 4/16 – PSA 5.3, Free-PSA 11.7% .
Week of 4/17 – The BIG WEEK – The week started with Houston being deluged in a 18+ hour period with anywhere from 10 to 20”s of rain, between Sunday evening, the 17th and around 12 Noon on the 18th. The result of all that rain was flooding in a number of areas of town. Irrespective of bayou widening and deepening, retention ponds and street drainage improvements that had taken place since the really massive flooding in 2001 caused by Hurricane Allison, Monday morning raising the garage door, I found my street under water and the water level about half way up the driveway. It continued to rise and by about 11:30 AM the water had reached the 2” rise of the garage floor above the driveway surface. Time to start move stuff on the garage floor to a higher location! Over the next 45 minutes I watched the water slowly rise, breaching the edge of the garage floor and then begin to seep onto the garage floor. A pool of water moved about 5 feet into the garage then STOPPED. Then the water began to slowly recede. The water never reached the level of the interior floor, which was 2” higher than the garage floor ! Well, after the concerns and excitement of Monday, the biopsy scheduled for Thursday wouldn’t be the highpoint of the week.
I’d decided to take before the biopsy a 500 mg tablet of Hydrocodeine Acetaminopen (a opioid pain medication) left over from a tooth extraction. With that tablet and a messenger bag containing packet of info on the nerve monitoring system, I headed into the Texas Medical Center for my 10:15 AM appointment. The traffic wasn’t as bad as expected, so I arrived in about 40 minutes, instead of an anticipated 60. After signing in I took the Hydrocodeine tablet then took a seat in an office filled will older men and their spouses. After a 30 minute wait my name was called by a young lady who indicated she was part of the biopsy team and would give me an antibiotic injection and fill out some additional paperwork. She asked if I had been taking the Cipro-based oral antibiotic as instructed (Yes) then asked me to drop my pants so she could give me an additional antibiotic injection in my buttock. Had I been taking any blood thinners (such as aspirin) in the past 5 day? I lied a bit with this question, as part of my daily morning regime is one 325mg aspirin. I’d not taken the aspirin this morning, but had taken aspirin on Monday, Tuesday and Wednesday mornings. I told her I stopped aspirin on Tuesday. She frowned upon hearing, saying I should have stopped earlier. She then proceeded to fill out a computer based questionnaire on my health history. When she came to the question – “are you sexually active” – I replied – “when the opportunity arises”, she let out a small giggle. Completing the preliminaries, she asked me to take a seat in a smaller waiting room, separate from the one I’d originally waited. She said the ultra-sound technician would call me in 10-15 minutes.
The ultra-sound technician told me he had been associated with the urologist group for about 15 years. He was going to help with the final preparations before Dr. B arrived to do the actual procedure. He asked me to undress and put on a hospital gown. He then explained what I’d experience during the biopsy. A lubricant jelly containing lidocaine would be squirted into the rectum to facilitate the placement of the ultra-sound probe and the sampling gun. He demonstrated how the firing of the gun would sound (kind of like mouse trap snapping shut). On a side table tray were 14 slides, each with a blue foam square. I assumed these were to keep some orderly arrangement to the location in the prostate where the tissue plug is taken. He asked me to get upon the gurney and helped position me (legs in fetal position towards the chest) resting on my left side, facing a wall. He said he would take some initial pre-biopsy ultra-sound images before he’d call for Dr. B. In went the lidocaine lube, the ultra-sound probe – the procedure had officially begun. He kept asking for me to tell him it if was uncomfortable or hurt. The ultra-sound images completed he briefly left the room and then returned saying that Dr. B would be here in a couple minutes.
Dr. B appeared, greeted me with a Good Morning. I greeted him back, asking if after the biopsy, would he have 5-10 minutes so I would talk with him. He said certainly. He then told me that he planned to take a standard 12 core sample and told me to tell him if I was experiencing any pain. The mouse trap noise and a momentary pressure felt – no pain. Was the lack of pain the result of the codeine, the lidocaine lube or was it just my high threshold for pain? Only once during the 12 mouse trap noise did I feel a slight pain/major comfort. During the procedure Dr.B remarked you’re not bleeding any – that’s good. The biopsy was completed in less than 10 minutes. (Compared to having a tooth extraction where that is a 10, this biopsy would rate maybe a 2 or 3 on the same pain scale.)
The biopsy completed, I rolled over on my back and started to sit up on the gurney. Dr. B told me to continue to lay back and he adjusted the head pillow to make me a bit more comfortable. He told me what to expect after the biopsy, regarding blood in urine and feces and to not engage in any sexual activity for the next 5-7 days. I then began a short conversation, indicating my professional background in medical device sales, discovering the nerve monitoring device in a YouTube video. He said it sounded like another Cavermap (a now defunk product which about 15 years ago was marketed to help the surgeon locate prostate –related nerves). I indicated the system was specifically designed to be used with the da Vinci system to locate the somatic nerves associated with continence and potency. He indicated he got pretty good surgical outcomes with patient results without nerve monitoring – I retorted that certainly the nerve monitor is not a substitution for a surgeons technical abilities, but I personally, after learning about the nerve monitor would not consider having prostate surgery without the surgeon using the monitor in my surgery. He paused a bit – then asked if I had materials on the monitor (he’d never heard of it before our conversation). I said there was a packet in my bag. He said he was an hour behind schedule this morning and couldn’t talk more. He asked me to leave the packet with his clinic nurse manager. He said he’d look it over and then perhaps I could stop by his office and talk more over coffee or a glass of wine. WINE ? Never heard that before! But then again, how many experienced urologists get a sales pitch from a patient after they have just given that patient a 12 core biopy ?
Dr. B left the room and the ultra-sound tech handed me a box of Kleenex and said I could clean up and dress; he would be back in a couple minutes. When he returned, I gave him the nerve monitor info packet and asked him to give that to the clinic nurse manager. We briefly talked about the MRI Fusion equipment in the room (which wasn’t used on my biopsy – because the MRI had been “normal”). MRI Fusion would allow the urologist to specifically sample loci of suspect cellular areas in the prostate which were revealed by the dye infusion portion of the MRI scan. In my case, with the MRI showing “normal” this couldn’t be used and so the standard patterned 12 core biopsy was used.
Dr. B had indicated I would probably experience blood in the urine and possibly stool which was spotted with blood. However, during the balance of the day, when urinating, there was not any suggestion of blood in the urine, nothing in the stool. Thursday evening upon urinating, there was a very slight suggestion in the first part of the urine flow of a reddish discoloration. Still I experienced no pain. I took another 500 mg of codeine before going to bed and had an uneventful sleep.
Friday morning, 4/22, I was bushing by teeth and looked down and saw a bright red liquid droplet on my left foot. Not having urinated yet, I looked at the tip of my penis. A squeeze produced another small red droplet. I realized this was blood, which not appearing on Thursday after the biopsy, had probably drained into the vas deferens, mixed with pre-existing seminal fluid and then eventually during the night moved into the urethra. My upright standing position and gravity had caused the mixture of blood and seminal fluid to leak out of the penis. I urinated and check the residual urine in the penis – no additional blood. I continued my morning plans. Having taken a “sick-day” for Thursday and Friday, I had some free time to attend to personal things not easily done on a weekend. In the afternoon back at the residence I had a bowel movement. During the bowel movement the associated urination produced a very large volume of a blood /seminal fluid mixture in voided urine. The mixture was heavier than water and didn’t disburse but sunk to the bottom of the toilet bowel. The bright red coloration against the white porcelain of the toilet bowel was a bit disconcerting – but still no pain. Other than the blood in the urine, the only other lingering post-biopsy feeling was a sense of a different “feeling’ in the rectal area. I assumed this was swelling of the prostate from the 12 punctures it suffered on Thursday morning.
Saturday, 4/23, I noted during the day some reddish circular stains in my boxers – suggesting that after urination, the urine dried and left the RBCs in the urine more easily seen against the white material of the boxers.
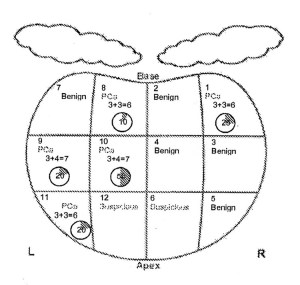
Week of 4/24 – On Tuesday the 26th the clinic nurse manager called and indicated that my biopsy results were available and asked me to come in on Friday, 4/29 to meet with Dr. B. Friday, 4/29, I arrived a bit earlier than planned because my calculations on potential traffic to the medical center overestimated the actual drive time – for the 11:00 AM appointment. About 11:15 my name was called and was directed to a examination room by one of the medical assistants. She indicated that Dr. B had just completed a robotic prostatectomy and would be here in about 30 minutes. At 11:45 AM there was a knock on the examination room door and Dr. B arrived with a folder containing my biopsy information. His first remark was – Well, it looks like I did too good a job with the biopsy. I told him that after the PCA3 results (the genomic test) coming up as positive for malignancy – the biopsy wasn’t a surprise. He pulled the pathology report out of the folder and began to discuss the results. The graphic of the prostate and sampled areas with the pathologist’s Gleason values are shown at the left. The “cloud-like” drawings above the prostate diagram are the vas deferens. There were 12 cores (samples) taken with the prostate being divided into 6 areas for each of the right and left lobes. My right lobe only had 1 core that showed a low grade malignancy (Gleason 3+3=6) The left lobe had 4 cores that showed malignancy. 2 of these were (Gleason 3+4=7) and the other 2 were (Gleason 3+3=6). There were 2 cores which were benign or “suspicious” but not falling into the standard Gleason scoring nomogram. Dr. B went on to indicate that the biopsy did not suggest that there were any breaching of the prostate wall by the malignancy. He indicated that his earlier DRE (digital rectal examination), the MRI and the pathology report would stage (classify) my cancer as T1c (tumor identified by needle biopsy because of an elevated PSA level). However, my own take on staging, I would fit into the T2 category (tumor confined within the prostate, found in 1 or both lobes by needle biopsy but not palpable or reliably visible by MRI.
Dr. B then went on to describe the therapeutic options which I needed to consider:
• Active Surveillance – Continued monitoring via PSA values every 6 months and possible additional biopsy, depending upon the PSA value.
• EBRT – External Beam Radiation Therapy – generalized radiation to the pelvic area (including the prostate) (Non-evasive procedure)
• Cryotherapy – Freezing of the cellular areas containing the malignant cells, leaving other areas of the prostate untouched (Semi-evasive procedure)
• HiFu – High Intensity Focused Ultrasound which heats the area of malignant cell area to 90 C = 194 F, leaving other areas of the prostate untouched (Non-evasive procedure)
• Robotic Assisted Prostatectomy – The da Vinci Robotic Surgical System – removal of the entire prostate, vas deferens and examination of associated lymph nodes for possible metastatic growth. (Evasive procedure)
During the discussion of the options – his cell phone went off and he excused himself from the room. He returned in about 10 minutes and apologized for the interruption. He said he had another robotic prostatectomy scheduled to begin at 1:00 PM and that was the OR wanting to know when he would be there.
Surprisingly he volunteered that he would use the nerve monitoring system on my surgery if I elected the surgical option. I asked if he’d reviewed the materials in the packet I’d earlier left with his clinic nurse supervisor. He said he hadn’t – but it was in his briefcase. I then provided him with another packet of different information – which he said he’d look at when he had time. I told him that in his options he didn’t indicated the Cyberknife. He said that fell into the general classification of EBRT – but he felt that the technology hadn’t been thoroughly published on in peer reviewed clinicals. I told him I was meeting on Tuesday, 5/3, with Dr.C to get his assessment (relative to the pathology report) of my suitability for Cyberknife therapy. I would then make a decision on either the da Vinci prostatectomy or Cyberknife therapy. I would let his clinic nurse know Friday, 5/6.

Saturday, 4/30, (9 days after the biopsy) I felt it was time to masturbate to relieve some of the prostate swelling I could feel when fingering the prostate. Selecting some suitable “stimulating” video material, my climax produced a cabernet-colored ejaculate. Perhaps a bit distressing in its look – but simply the results of the 12 biopsy cores and prostate’s internal bleeding – something I’d expected to see. If I’d ejaculated sooner than 9 days, the ejaculate would have probably been a bright red instead of the darker Cabernet color.
May 2016
Week of May 1 – On 5/3 I met with Dr. C at the Cyberknife facility. He had seen a copy of the pathology report because I’d e-mailed it to him on Friday after meeting with Dr. B. I told him that I assumed my biopsy put me into the low or low-intermediate “risk” group of patients (a radiology oncology ranking based upon the Gleason score on the core pathology. He said I was correct and was a candidate for Cyberknife therapy. He again went over the treatment schedule – placement of 4 or 5 gold fiducials in the prostate, injection of the SpaceOAR hydrogel between the prostate and the rectum, initial CT scan to make sure of acceptable fiducial placement, 2- 5 day wait for the fiducial placement to stabilize in the prostate, pre-treatment MRI and CT scan slices for organ mapping and dosimetry planning, fitting to a customized body positioning cast and then finally the 36.25 Gy (Grays) of radiation divided over 5 sessions separated by one day (exclusive of weekends). He pulled up another patient’s CT scan which showed how the fiducials appeared. He said I could think it over and tell him later in the week or next week. I said that wouldn’t be necessary – after reviewing the pros and cons (relative to my personal situation as a single man ) in my mind it’s Cyberknife and not da Vinci robotic surgery. He said – Well if that’s the case, I’ll get my staff to order in the fiducials and the SpaceOAR on Wednesday. He wanted to know what my schedule was – I indicated I had an appointment with a urologist regarding the nerve monitoring system on Thursday, 5/5 – but after that I’d made sure that the balance of my May was open. Friday, 5/6 Dr. C’s nurse calls indicating that the fiducials had arrived and Dr. C would like to schedule their placement for 5/10. She indicates that because of recent “controlled substance” regulation from DEA, she can’t phone in the prescriptions to my pharmacy for the hydrocodone / acetaminophen, 5mg/325mg (codeine to dull the pain response) and an antibiotic ciprofloxacin ( i.e.Cipro, 500 mg) I needed to take before the procedure, as well as the 12 hours after to minimize infection from the procedure. I told her I’d come by the Cyberknife facility on Monday, 5/9 and pick up the prescription.
Having indicated to Dr. B that I’d have a decision on my treatment selection by Friday, 5/6, I spend that Friday afternoon composing an e-mail to be sent to him, via his clinic nurse manager’s e-mail. I wanted to be frank with him, yet word the e-mail carefully so that his professional standing in the Houston urology community would not be slighted, as I hoped to continue to work with him relative to the nerve monitoring instrumentation for the da Vinci Surgical System.
When we met last Friday, 4/29, I told you I’d have a decision by today, regarding my selection of the therapeutic intervention for my biopsy-based diagnosis of prostate cancer.
Considering the best options available to me – da Vinci prostatectomy, done by an experienced surgeon OR stereotactic body radiation therapy (SBRT) – i.e. Cyberknife, my decision is to select the Cyberknife option.
As with many of life’s choices, my selected choice is colored by factors not necessarily related to the issue requiring the choice. In my case, these boiled down to 4 areas of concern.
• Recuperative Time – Post Procedure
I am a single man. While I have a supportive network of friends here in Houston, none of those individuals would be available for day-to-day (in residence) assistance over the 2-3 week surgery, post-operative period. While I earlier had contacted a Houston home-healthcare group about in-residence assistance, its cost, while not prohibitive, would not be required when using SBRT.
• Age and Outcomes – Biological Failure Rates
At age 64, while I am in good health, the thought of a 2-3 week post-surgery, recuperative period is something I’d prefer to avoid if possible. While clinical papers are always subject to discussion, my reading of both da Vinci and Cyberknife papers cite PSA / biological failure rates that are quite comparable at 5 years. The only difference is with da Vinci the PSA value drop immediately after surgery (the offending organ has been removed) while with Cyberknife the PSA value exhibits a logarithmic decline over a period of 12-24 + months.
• Procedure Impact On Urinary Continence and Sexual Potency
Of those two conditions – while both (even at 64) are important to me, continence vs. incontinence is the most important. While the use of the nerve monitoring instrument in conjunction with the da Vinci system should significantly reduce the time to return to full continence, there are no surgeons in the greater Houston/Galveston area who have yet to incorporate this nerve monitor into their robotic prostatectomy procedures. I greatly appreciate your indication that you would use the nerve monitor with my surgery – however the two earlier discussed issues (above) were seen as more important in my final decision. Additionally, clinical literature on Cyberknife indicates that urinary incontinence is typically not reported in the SBRT therapy.
• Procedural “Toxicity” – Surgery vs SBRT
In our conversation of the 29th, you indicated that only once had you nicked the intestine and that was resolved with a tissue patch for closure. With any type of radiation there is always the risk of tissue damage to close lying, surrounding tissue. In the case of SBRT therapy, radiation toxicity to the rectum is a concern. In my selection of Cyberknife therapy, that decision was made easier by knowing that a newly developed, biodegradable, injectable hydrogel material – SpaceOAR – would be used in my therapy. SpaceOAR provides around a 1.0cm separation between the prostate and the underlying rectal mucosa. SpaceOAR, in limited clinical studies, has shown to essentially eliminate the risk of rectal toxicity when used in conjunction with Cyberknife therapy.
In closing – I’d like to add a few personal comments and observations.
Irrespective of my decision to use Cyberknife therapy instead of da Vinci surgery – I recognize your significant experience with the da Vinci system and your obvious technical acumen in providing your prostatectomy patients the best current “standards-of-care”. Your highly successful transition from open procedures to robotic procedures suggests your openness to further enhance those “standards-of-care” through the incorporate of real-time nerve monitoring during prostatectomies. While I will not be seeing you directly as a patient – I would hope that you will consider adding the nerve monitoring instrumentation to your da Vinci robot at the hospital. It would be my honor to help facilitate your evaluation of the nerve monitor in the next 30-60 days.
The other observation relates to the current post-biopsy patient information packet, provided during the patient pathology report review session. As a potential patient with a 25+ year professional background in healthcare marketing I was a bit surprised at the patient packet I was given by your staff. I won’t go into details here, other than to say a folder containing Xerox pages of multiple prior Xeroxed pages took me by surprise. Additionally, there was no mention of the da Vinci surgical system that would presumably be used for the patient’s prostatectomy. In fact the 6 page Xerox entitled “Information for Patients After Radical Retropubic Prostatectomy” seemed to be more suggestive (in parts) of an open procedure than a robotic one. With my professional background in marketing, the opportunity to work with you to update your patient information packet would be an honor. I extend this offer to you – as a cost-free decision, irrespective of your decision about the nerve monitoring system.
May 2016
Week of May 8 – Having picked up the prescriptions on Monday, and having followed the instructions for intestinal gas reduction (BeanO) over the weekend and prior clearing of the bowel (fleet enema) before leaving for the appointment of 5/10, I arrived at 8:00 AM to the Cyberknife facility. Around 8:30 a man passed through the waiting area rolling a strange multi-bracketed device (I later would find out that was the positioning device for the ultrasound probe). This was then followed by a more equipment which I recognized as the ultrasound equipment. Around 9:00 Dr. C’s nurse opened the door and called me – taking me to a room which was a combo changing room and rest room. She asked me to change into a hospital gown and put my clothes in one of the lockers in the room. Completing that I went into the hallway across from the room where the procedure would take place. The nurse directed me into the procedure room and asked me to get up on the table which was looked to be a slightly modified gynecological table with leg stirrups. As she left the room she indicated that Dr. C. would be there in a few minutes to place a topical anesthetic (lidocaine) that would set for about 30 minutes before additional lidocaine was injected into the perineum (between the anus and the scrotum). Unlike the earlier biopsy of the prostate, where the prostate tissue samples were taken by a needle passing from inside the rectum, through the rectum wall and into the prostate, the gold fiducials are placed into the prostate by needle access outside the body through the perineum space between the anus and scrotum. Both types of procedures would use trans-rectal ultrasound, abbreviated as TRUS – in that the ultrasound probe is placed in the rectum to facilitate the visualization of location and placement of either the biopsy core sampling, or this morning to visualize the needle containing the fiducials as it enters the prostate and deposits a fiducial. Dr. C arrived with his nurse, cleaned the perineum area with a antibiotic scrub and then applied a lidocaine gel to the area where the injections would occur and then overlaid that area with a membrane patch to minimize re-contamination of the cleaned and lidocaine jell area. Dr. C said he’d be back in about 30 minutes.
It was more like 40 minutes when Dr. C and his nurse returned – his time to do the lidocaine injections into the perineum area. Apparently the prepared syringes for these injections required some additional medications mixed with the content of the syringe. It was difficult for me to determine the number of injections because of the prior lidocaine-numbed skin – probably no more than 4 separate injections. Dr. C indicated he’d let the injections take effect before beginning the first part of the procedure – the fiducial placement. About 15 minutes later Dr. C, his nurse and the man I’d seen earlier with the ultrasound equipment entered. Dr. C. introduced the man as the ultra-sound expert who would be assisting him in the fiducial and SpaceOAR placement.

The multi-bracketed device I’d seen earlier was the holder for the ultrasound probe. The ultrasound technician asked me to move a bit forward on the examine table so that the probe and its bracket would be better aligned with my anus. The probe was a black, and appeared to be about 7” in length and no more than 1” in diameter. The technician covered the probe with a condom and Dr. C lubricated the condom to facilitate it’s placement in the rectum. Once the technician had acquired a good image of the prostate he fixed the probe holder and indicated Dr. C could begin the placement of the first 2 fiducials. (A photo of a solid gold fiducial, like was used in the procedure is shown at the left.) The placement of all 4 fiducials when smoothly without no more discomfort than I’d experienced with the prostate biopsy. The ultrasound technician and Dr. C continual communicated during the process, the technician acting somewhat like a “back-seat” driver, making comments on the needle location relative to the prostate area where the fiducial would be injected into the tissue.
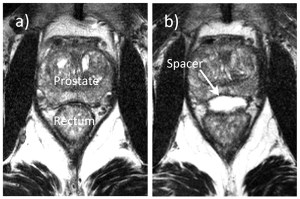
The placement of the SpaceOAR hydrogel is a bit more complicated. The material is similar to the dermal fillers used by aesthetic cosmetic surgeons to fill in depressions or wrinkles in facial features. It is biodegradable so the original volume is absorbed by the body over a period of 6 -9 months. SpaceOAR was recently approved by the FDA (April 2015) for use in urological radiation oncology. The material is injected between the rectal wall and the prostate to widen the separation between those two tissue areas, significantly reducing the possibility of radiation injury to rectal tissue during stereotactic body radiation therapy (SBRT). The following images are from a clinical showing a MRI scan of the prostate area before (a) and after (b) in the placement of the SpaceOAR hydrogel.
While Dr. C was preparing the hydrogel mixture, the ultrasound technician repositioned the probe to better visualize the area where the SpaceOAR would be injected. He commented to me – you have a really nice fatty layer between the prostate and rectal wall. I replied back – I guess that is a compliment? He just smiled. I knew from my research on the placement of SpaceOAR that prior to the hydrogel placement saline is injected into the fatty layer I’d just received a compliment about. This saline injection “opens up” the fatty space, creating an area where the hydrogel can easily be subsequently injected.
While having had minimal discomfort from either the biopsy or fiducial placement, I expected that the SpaceOAR placement would be similar. I was mistaken – for as soon as Dr. C began the fatty tissue layer saline injection I experienced a sharp pain that caused me to grimace. Dr. C’s nurse sensing my pain/discomfort, patted me on the shoulder and suggested I start breathing in a “Lamaze” technique, which should help reduce the discomfort. The saline separation completed, while the needle was still in place, Dr. C connected the hydrogel mixing syringe to the needle. Under guidance from the ultrasound image and the technician he injected the SpaceOAR into the now separated space between the prostate and rectum. Throughout this procedure I continued to experience discomfort and occasional, brief shooting pain. So far, in all the procedures this was the one with the most discomfort or pain. Perhaps the hydrocodone had begun to wear off as it was now about 2.5 hours after I’d taken the 5mg tablet. However, the fact that the pain was transient and brief would not have recommended Valium sedation or any more involved anesthesia. The whole process took about 2 hours to complete.

I next was moved by wheel chair to the CT imaging room. There the position of the fiducials and Spacer OAR was quickly scanned. Dr. C deemed the placement of the 4 fiducials as excellent. These fiducials will serve as permanent internal markers for the positioning of the Cyberknife, assuring that each treatment session is identical to the prior session. . The X-ray image shows the 4 fiducials (circled in red) as they were placed in my prostate on 5/10. I left the Cyberknife facility and treated myself to a lunch of Gulf oysters on the half shell and a cup of seafood gumbo on the way back to my residence. The balance of the day was spent with some business paperwork, then a light dinner, shower and early to bed about 9:00 PM.
The next morning, Wednesday, 5/11, I awoke feeling like I was beginning to come down with a cold – a bit of aches and pains – but no fever. I really felt being “under-the-weather” for most of Wednesday. For lunch I went out to Chick-Fil-a and then for dinner had a bowl of Chicken-noodle soup (a tried and true remedy I fall back on when feeling like a cold is coming on). I took a really hot shower and when to bed about 8:00 PM. I wondered if this was an immune (foreign body) reaction to the SpaceOAR injection. The product literature and clinical publication on the product didn’t indicate any reaction of that type to the hydrogel. Thursday morning – 5/12, I awoke without the symptoms of Wednesday – the Chick-noodle soup worked ! I dropped Dr. C a short e-mail indicating I had experienced a 24 hour period of what felt was some type of an immune reaction. He replied he’d not had that reported by any prior patients but had gone ahead and reported it to the SpaceOAR company – Augmenix.
When I felt the rectal area of the prostate, two days after the procedure, what I now felt was a rectangular area with a defined shape and edge/ridge that was hard to the touch – the area of the SpaceOAR hydrogel. It seemed quite immovable upon touching, so I wondered how the SpaceOAR would interfere with normal bowel movements? That’s all one needs is a bowel obstruction that won’t go away for 6 + months !
Week of 5/15 – Monday, 5/16 I received a phone call from one of the staff nurses at Cyberknife, indicating that they would like to schedule the Cyberknife planning CT and MRI scans for Thursday, 5/19, essentially 10 days after the SpaceOAR gel and fiducial placement had occurred. The staff person said I should prepare for the CT and MRI scans in the same manner which I’d prepared for the earlier fiducial and SpaceOAR procedure. Easy enough !
Thursday, 5/19, arrived around 10:30 AM for the 11:00 CT scan. Shortly after 11:00 the senior radiation tech and her assistant met me in the waiting room and asked me to follow them back to the CT scan area where 10 days earlier I’d had a short CT scan to validate the placement of the fiducials and SpaceOAR hydrogel. They asked me to change into a hospital gown and indicated that part of the CT planning scan would require them to place a Foley catheter in my urethra. This would allow specific and accurate measurements of the urethra thickness and path it took through my prostate. They would also be making a body cast of me that would be used through the CT, MRI and Cyberknife procedures. This would provide some added assurance that the position of my body was always in a close approximation to where it was during the CT and MRI scans which would be done this morning. The body cast (Vac-Lok™) is filled with what seemed to be some type of polystyrene beads, similar to what one might see in a “bean bag” chair. As I lay on the transport table of the CT scanner, with the Vac-Lok cushion under me, the two nurses positioned my legs and torso and pulled the cushion up around the sides of my torso and under arm area. They then started a vacuum pump and the semi-soft cushion became a more rigid form. According to the manufacture of the Vac-Lok system, when the air is evacuated from the cushion, the cushion will retain the body imprint over the duration of the radiation procedure and can be reused (if necessary) and reconfigured to another patient by release of the vacuum. Next came the insertion of the Foley catheter. The senior radiology technician had been with Dr. C for 15 years the other was a new hire. The new hire placed the Foley with the supervision from the senior technician. Although I’d urinated prior to coming into the CT scan area, the Foley drained additional urine from my bladder into a bowl which the nurses had placed between my legs. After the flow became a “drip”, a plastic clamp closed off the Foley, the bowl was removed and the two techs left the CT room so that the CT scan could begin. The scan would cover an area from mid-abdominal to mid-thigh. After a quick scan that lasted about 5 minutes, both technicians came back into the CT area; the senior technician and said I had too many “gas” pockets in my intestine and some residual feces. They could not make an appropriate planning scan. The senior technician questioned if I had followed the suggested preparations and taken BeanO to minimize gas. I told her I had done the same prep as I had done for the fiducial and SpaceOAR procedure. She said well, it apparently wasn’t as effective this time as before. Bottom line, they would have to reschedule the CT / MRI and hope that next time my “gas” wouldn’t be a problem.
The senior radiology technician wanted to know if I wanted to meet with the nutritionist, who had been scheduled for me to see that day. I said I’d like to get that out of the way, while I was there. I dressed and returned to the waiting room and indicated to the receptionist that I was there to meet with the nutritionist.
The nutritionist appeared in a few minutes and I went with her back to a small conference room. She asked some basic questions about appetite, maintaining weight and hydration during the Cyberknife treatment. I told her that my scheduled CT / MRI scans of that day had been cancelled as my “prep” for the procedures had not been sufficient. It was then I learned from the nutritionist what I should have done in the way of “prep” was not what I actually did. She asked – Didn’t you get the outline ? No, I replied. She said let me get you a copy and left the room. When she returned, briefly looking at the document described a much more rigorous prepping than I had done – in fact the procedure prior for CT / MRI scan planning was more like that used for colonoscopy preps. I told her obviously, I had fallen through the cracks when it came to being give patient materials. She indicated that was unfortunate and she would make sure the oversight was discussed at their weekly staff meeting.
The nutritionist went on to explain some of the food do’s and don’ts for the preparation. She gave me a 8 oz. bottle of a Ensure “Clear”, which is a protein drink. She indicated that the main thing going forward with Cyberknife treatment is to reduce bowel bulk volume and bowl gas. Leaving the meeting with the nutritionist, I returned to the reception desk where the senior radiology technician was looking at the schedule for the facility’s “open” MRI system. It looked like the earliest date / time available on it would be Friday, 5/27 at 8:00 AM. That day/time was booked for the MRI and the senior radiology technician indicated I needed to be at the Cyberknife facility at 7:00 AM that morning so that the CT scan could be completed (hopefully) with success, before the MRI.
Returning home I was a bit pissed off, for not earlier being given the information on the detailed “prep” for the CT / MRI scan. That meant that the start of the Cyberknife therapy was postponed by at least 7 days. My assumed completion of therapy, sometime during the week of June 5th, now became the week of June 12th.
Later that evening I took time to review the Cyberknife “prep” document. As I didn’t want to have a repeat of what happened on Thursday and the “prep” was similar to that used for colonoscopy, I found a colonoscopy prep document from the Medical Clinic of Houston website. It involved a divided dosing of a mixture of MiraLax and Gatorade taken the day before the colonscopy procedure. Having once prepped for a colonoscopy about 12 years ago, I remembered how complete the bowel evaluation was – this would surely give me a A+ rating by the senior radiology technician on the 27th.
Friday, 5/20, with shopping list in hand, I went to purchase the Dulcolax, MiraLax, Gatorade, 12 bottles of Ensure “Clear”, 2 cans each of Chicken broth, Beef broth. Shortly before 12 Noon I called the Cyberknife facility and talked with the senior radiology technican. I apologized for the lack of prep on Thursday and the inconvenience I may have caused by it – both for her and for me. I told her I now had the complete procedure prep documents and had decided that I’d simply do colonoscopy prep for the 27th to minimize a repeat of what occurred on Thursday. She said that she had learned that I had not been given the prep document and apologized for the staff not providing me information prior to the 19th. Saturday, 5/21, I had an e-mail from Dr. C – indicating that I had too much gas in the intestine for the CT scan. He indicated that he felt that doing a colonoscopy prep was a bit “severe” and that the outlined document which I’d earlier received a copy would probably be sufficient. I wrote him back that I didn’t want to have a repeat of the Thursday session and unless he felt it was ill advised, I planned to do colonoscopy prep for the CT/ MRI session on the 27th.
Week of 5/22 – Wednesday, 5/25, started the “prep” at 1:00 PM with 3 Dulcolax tablets, followed at 3:00 PM with half of the mixture of 64 oz. of Gatorade mixed with a 238 gram bottle of MiraLax. The routine suggested spacing the Gatorade in 8 oz. glasses every 15 minutes until 32 oz. had been drunk. The Gatorade/MiraLax mixture just tasted like Gatorade so it wasn’t difficult to drink – just a lot of liquid volume. The results of the purge began about 1.5 hours later and lasted intermittently until about 7:00 PM. Not having eaten anything since lunch I fixed a bowel of beef consomme’ and pondered whether I should finished the described “prep”. The colonoscopy indicated that at 9:00 PM on should drink the other 32 oz. of the Gatorade/Miralax mixture and taken 3 more Dulcolax tablets before going to bed. I thought, that’s all I need is having an urgency at 11:30 PM and not being able to make it to the bath room in time ! Since the CT / MRI scans weren’t until Friday morning, I decided to put the balance of the Miralax / Gatorade mixture in the refrigerator and repeat the process on Thursday using the remaining 32 oz. Thursday, 5/26, had a breakfast of plain yogurt, Jell-O and coffee. At 1:00 PM started the same procedure as on Wednesday. By 7:00 PM with only passing a liquid – I felt that if there was any major fecal material remaining in the intestine, it was minimal. However, I was still concerned about intestinal gas – which apparently plays havoc with not only ultra-sound imaging but also CT scan imaging. But, there was not much one could do about the gas, if it hadn’t been expelled as a flatulence. Around 10:00 PM I set the alarm for a 4:30 AM wake-up and went to bed.
Friday morning, 5/27, it was raining heavily when the alarm went off. I completed the “prep” by using a flee enema that resulted in no additional fecal material being expelled. One was not supposed to have any liquids after 9:00 PM on Thursday, so I brushed teeth, showered and dressed. Because it was raining, I decided to leave the house earlier than planned just in case there was a traffic problem on the way to the Cyberknife facility. Instead of an anticipated 45 -60 minute drive, the drive only took about 30 minutes. . At 6:20 AM the parking lot area of the Cyberknife facility was empty. I caught up on the Friday news using my iPad. About 6:55 AM I walked over to the automatic doors to the facility and while there was light from the reception room, there was no one at the desk area. I jiggled the door a bit – nothing. Humm, here I am all prepped and read to go for the 7:00 AM appointment and the place is locked. I decided to go back to the car and call the senior radiology technician (whose cell # I’d gotten just in case I found the doors locked at 7:00 AM). Half way back to the car the facility door opened and a lady called, wanting to know if I was their 7:00 AM appointment.
Returning to the facility, I was met by the junior radiology technician who indicated I needed to take off my street clothes and change into a hospital gown. Doing that, I then met the senior technician who took me to the CT room. The body form cast was in place on the CT gurney. It was like cement! What earlier had felt like a bean-bag pad with the complete evaluation of air from the pad resulted in an extra hard body impression. I asked that a pillow be placed under me where the body cast ended and the gurney surface began. This helped considerable in making the cast more comfortable. I told the technician that while I was sure there was little fecal material left in the intestine – I was still having gas anxiety – hoping that was not going to be a problem this Friday.
The senior radiology technician said they were going to do a preliminary scan to check on how well the “prep” had worked. The CT gurney moved me into the CT scanner and 5 minutes later moved me out. The senior technician returned indicating while I had some gas in the upper intestinal track, the lower track in the area of the prostate was clear of both gas and feces. They could proceed with the CT scan.
As the CT scan doesn’t clearly show the walls of the urethra, a Foley catheter was inserted before the scan began. Image measurements taken from the CT scan will then be used for the planning of the Cyberknife sessions. CT derived measurements of the prostate, urethra, bladder and intestine, relative to the location of the 4 gold fiducials, are very important to the success of this therapy. The irradiation from the Cyberknife is very precise so as to only irradiate those areas of the prostate which contain the malignant tissue. The urethra and areas surrounding the prostate are spared the same level of radiation that is received by the prostate tissue itself.
The CT scan took about 20 minutes and the senior technician indicated they looked beautiful – quite satisfactory for planning measurements. Before I got out of the body cast, the technician made a “X” with a black magic marker on my right and left thigh at the level of the hip socket. She said this was for making sure my position in the MRI was the same as it had been in the CT, The senior technician said I could get dressed back in my street clothes and go across the parking lot to another building where my MRI would be done. She said they would follow in about 15 minutes with the body cast.
Arriving at the MRI facility and signing in – I was met by the MRI technician and directed to an area where I would change to a hospital gown. I could keep my underwear (boxers) on for the MRI. Returning to the hallway in my gown the MRI technician indicated they would be doing a contrast dye injection (gadolinium) and so needed to place a cannula in my vein before they started the scan. He pulled a blanket out of a warming oven and covered me with a toasty 130 degree F wrap. The venipuncture /cannula placement completed I was taken to the MRI room where the senior CT / Cyberknife technician had brought the body form cast. The MRI was one of the new “open” MRI designs. Supposedly its design results in a lessoning of claustrophobia. The body form was already in place on the MRI gurney. I got into the body form cast. It took about 10 minutes for two MRI technicians to adjust the height of the gurney relative to the available MRI spacing. The senior CT / Cyberknife technician double checked the “X” on my right and left thigh to make sure the positioning was correct. The MRI technician brought in some ear plugs and a headset that I could use to minimize the noise of the MRI during the scan. I requested some classical music – he said they used the internet program – Pandora. The MRI technician left the room and after a couple minutes the MRI gurney began to move me into the MRI.
Once I was inside the MRI, it seemed that calling it an open MRI was a bit incorrect. While the sides of the instrument were open, my nose was about 2 inches from the upper wall of the MRI interior. (This was later explained that because of the body form cast, the normal body positioning was elevated 6 to 7 inches higher than normal. For most MRI scans ones nose wouldn’t be almost rubbing the upper wall of the MRI.). I’m not sure why they supply music and head phones during these procedures, as the noise associated with the magnets of the MRI was very, very loud – essentially drowning out any music that might be coming through the headphones. This open MRI seemed to be much more noisy than the traditional donut MRI design which was used in my pelvis scans back in February. After about 40 minutes into the MRI scan, the noise stopped and the MRI technician returned. He said I was just doing great with staying still during the scanning. He would now inject he gadolimium for the dye contrast enhancement scans. He asked me to place my left arm with the cannula on an arm support which he attached to the gurney. (Now I could see the advantages of the open MRI – injections can be done without moving the patient’s position – as the open design allowed for the patient’s arm to be easily accessed). Having injected the gadolimium he left the room. About 2 minutes after he left the room I experienced a series of coughs. I assumed it was some type of reaction to the injection. The coughs caused my upper body and head to move (but luckily I didn’t’ strike the inner wall of the MRI). The dye contrast enhanced scans took about 15 minutes more to complete. The MRI noise stopped and three MRI techs entered the area., The primary tech withdrew the cannula from the left arm and tightly wrapped a compression bandage over the needle entrance. He cautioned me about possible bleeding through that site. He said the scans went fine and I could get dressed now. I could leave the MRI facility. The whole MRI process took about 1.5 hours. I indicated that I needed to return to the Cyberknife facility to check what the schedule for the treatment s might be.
Back at the Cyberknife facility, I asked to speak with the senior CT / Cyberknife technician. She came to the reception desk and we discussed the start date for the 5 Cyberknife treatments. I had assumed that once the CT and MRI scans were satisfactorily completed things would progress rapidly. However, I was told that the radiologist generally takes about a week to complete the measurement and programming of the Cyberknife. As I will need to again be on a low residue diet during the treatment, I would like to know when I needed to begin that diet regime. The senior technician indicated that she assumed the first session would be on Wednesday, 6/8 and conclude on 6/17. I left the Cyberknife facility a bit too early for lunch – so I decided to grab a fish sandwich at McDonalds and then grill a beef filet for an at home celebration dinner.
Week of 5/29 – As the Cyberknife session will require about 1 week’s planning, there’s not much one can do except await a confirmation call as to when the sessions will begin. By Friday afternoon, I’d still not received a confirmation of the start date – so began the low residue diet and Milk of Magnesia evening dosage of 45ml on Sunday evening, 6/05, assuming that as the senior Cyberknife technician had indicated the first session would be on Wednesday, 6/8.
June 2016
Week of 6/05 – Not having heard from the senior Cyberknife technician or Dr. C regarding the start of the sessions, I called the Cyberknife facility Monday morning at 9:00 AM. The senior Cyberknife technician indicated that she was about to call me when I called. Dr. C had completed my treatment plan and they wished to start the Cyberknife sessions on Tuesday, 6/07 at 9:00 AM with a second session on Thursday, 6/09 and then three sessions on June 13th, 15th and 17th (Monday/Wednesday/Friday). Good that I started taking the Milk of Magnesia on Sunday evening, 6/05. (A screen capture of part of my irradiation session planning software image is shown below.)

Arriving at the Cyberknife facility Tuesday morning, I changed into a hospital gown, leaving on my boxers and T-shirt. The senior Cyberknife technician greeted me and took me into the Cyberknife area. She asked if I had any special music request and she would select a CD to play during the projected 40 minute session. I suggested something classical. She positioned me in the very rigid half body case, gave me a circular padded plastic loop for me to hold with both hands, positioned in my upper chest area. The CD music started (Mozart) and she left the room.
The Cyberknife sessions are planned using the four (4) gold fiducials that were earlier placed in my prostate (see the earlier X-ray image). Their specific locations in a 3-dimensional matrix are used as marker guides for the movement of the Cyberknife. The CT scan which had been done on the 27th, provides the image for very exact measurement of anatomical details and the distances between them and the gold fiducials. The software which controls the movement of the Cyberknife head uses those measurements to direct the angle of the head and the duration of the X-ray irradiation to a particular anatomical area of either the prostate or surrounding tissue (margins). While the irradiated area is determined down to 0.5mm, there is some radiation “scatter” that is created by either the tissue or bone which is in the path of the radiation beam. In the treatment of prostate cancer, the use of the SpaceOAR hydrogel to separate the prostate from the underlying rectal wall minimized irradiation to the rectum. However, the SpaceOAR doesn’t fully eliminate the scatter irradiation to the bowel and rectum, which will occur in the treatment sessions.
The session began with the gurney on which I lay shifting, making some position adjustment and then a couple of X-ray images being taken to confirm the positioning of the gold fiducials relative to the treatment plan images. The Cyberknife head began to move slowly to a position, stop, irradiate for a calculated time period (which is only seconds in duration) and then it would move to another location, pause, irradiate and move to the next programmed location. This continued for about 40 minutes, with pauses for gurney repositioning and additional X-ray positioning confirmation. You can view an abbreviated video of one of my Cyberknife sessions on YouTube at (https://www.youtube.com/watch?v=keWb1mVh_4I&feature=youtu.be). The initial session ended, the senior technician re-entered the Cyberknife area and helped me out of the half-body cast. She said I did really well during the session (referring to the fact that I didn’t move around much) and said she’d see me on Thursday.
Leaving the Cyberknife facility I thought that the most tedious part of all this will be the low residue diet, the 45ml of Milk of Magnesia the evening before the next Cyberknife session and the fleet enema the morning of the session to assure that the lower bowel and rectum area is devoid of fecal material and intestinal gas.
The Thursday session was a repeat of the initial session, requiring about 40 minutes from start to finish.
To celebrate a bit, since I had a 3 days weekend break until the next session on June 13th, I decided to break the low residue diet and have a well-deserved lunch at my favorite sea food restaurant in Houston – a dozen Gulf oysters on the half shell , a cup of seafood gumbo and a couple glasses of white wine.
Week of 6/12 – Sunday afternoon at 3:00 PM I began preparation for the week’s schedule Cyberknife sessions. Because I’d not been on a low residue diet Friday and Saturday of the prior week, I decided to again go through a colonoscopy prep, as had been done in late May for the planning CT and MRI scans.


The three Cyberknife sessions of the week went just as smoothly as the two of the prior week. Each were about 40 minutes in length coupled with music by Wolfgang Amadeus. On Monday after the session I took a photo of the Cyberknife control area the senior technician took a photo of me standing with the Cyberknife. (I learned from the senior Cyberknife technician that while not having a name, the facility’s Cyberknife is definitely of the “feminine” persuasion and likes on many days to be pampered). On Wednesday I use a GoPro Hero 4 Black camera to record the entire Cyberknife session (which was about 1 hour induration) in 1080P HD video. The shortened video, 12 minutes in length can be seen at (https://www.youtube.com/watch?v=keWb1mVh_4I&feature=youtu.be).
One of the potential side effects of the irradiation to the intestine is loose stool or diarrhea. However, as I was dosing with Milk of Magnesia every other day, as part of the Cyberknife preparation, it was impossible for me to know if I the loose stool and watery diarrhea I was experiencing was from the irradiation or the Milk of Magnesia. I’d have to assess that after the Cyberknife sessions ended on June 17th.
Before leaving the Cyberknife facility on Friday, 6/17, I met with Dr. C’s nurse and Dr. C himself. A nurse did a post-treatment session exit interview with vital signs and then Dr. C briefly met with me to discuss the next step in monitoring the success of the Cyberknife sessions. I will need to have a PSA drawn in about 6 weeks and the results forwarded to Dr. C. for the follow-up consultation which they’d scheduled for August 12th. After the nurse left the examination room, I asked Dr. C if I could talk with him before leaving. I closed the door so that the nurse and staff would not hear my comments. I told Dr. C that I had nothing but high praise for his staff and particularly the senior Cyberknife technician who shepherded me through the 5 session over the past 10 days. I told him that comparing the Cyberknife staff and sessions to my urologist’s staff would be like comparing a visit to a Lexus dealership to purchase a car (i.e. Cyberknife) to shopping the lot at a used car dealer (i.e. the take-a-number and wait feeling from the staff and the rush/rush of the over-booked urologist who wished he had more time with you, but had to rush on to see the next patient). Dr. C simply smiled and said they try to make the patient experience at the Cyberknife facility a good one.
Week of 6/19 – No longer taking Milk of Magnesia every other day I was now able to assess the impact of Cyberknife irradiation to my lower intestine. As of 6/22 I was still experiencing a loose stool and feeling an urgency to defecate a number of times during the day. Occasionally, in wiping after defecation, there would be a faint trace of blood. As the voided stool showed no signs of blood, I attributed the trace of blood to the rectal tissue around the anus, where I felt some slight irritation from all the prior Milk of Magnesia induced voiding. I started to use an Aloe Vera jell as an anal suppository to help heal the tender tissue of that area. There was some slight burning associated with urination and an intermittent urine stream that was more pronounced than prior to the Cyberknife sessions. However the urinary changes were minimal and were also expected, as the urethra runs directly through the middle of the prostate and received a significantly high cumulative dose of irradiation during the 5 treatment sessions.
Week of 6/26 – Towards the end of the prior week, I began to feel “bloated” with some discomfort in the abdominal area. As my stool over the week of 6/19 had largely consisted of small pieces of feces, sometimes formed, sometime loose, I felt that there was an intestinal backup of digested food creating the discomfort. Sunday evening I took 45 ml of Milk of Magnesia, assuming that would help to clear up the intestinal problem. Monday morning there was still no relief and I felt even more bloated. This was a bit troubling – what if the radiation scatter had impacted the small intestine, perhaps causing an impairment of the bowel motility reflex or even more serious tissue damage and some adhesions of the intestine ? I decided to reinstitute the colonoscopy prep procedure before contacting Dr. C about my concerns. I took 3 Dulcolax pills at 9:00 AM and preparing the Gatorade/Miralax mixture to take around 3:00 PM if the Dulcolax pills didn’t show signs of acting by that time. (The Dulcolax box promised “gentle, dependable relief in 6 to 12 hours.) 6 hours later at 3:00 PM there had been no urgency for a bowel movement – only the continued bloated feeling. At 3:00 PM I took the first 8 oz. glass of the Gatorade/Miralax mixture. I’m not sure if this triggered the Dulcolax action but about 15 minutes later I had a significant bowel movement. I decided to suspend the continued drinking of the Gatorade/Miralax mixture. The initial bowel movement was followed about every 20-30 minutes with a smaller movement over the next two hours. If there had been an obstruction – it had been cleared. The balance of the week of 6/26 there were no further bowel movement problems and it seems that issue has been successfully resolved at this time.
July 2016
Week of 7/04 – Two weeks have now passed since the last Cyberknife session. Urinary function is back to the pre-Cyberknife “norm”, bowel movements are back to “norm” and sexual function seems intact, however the volume of seminal fluid is much less when ejaculation occurs. (The decrease in seminal fluid was expected as the Cyberknife session irradiates the entire prostate, disrupting the function of both malignant and non-malignant prostate cells.)
August 2016
Week of 8/01 – The six week PSA post-Cyberknife value is 2.6 ng/ml. This is contrasted to the pre-biopsy PSA value of 5.3 ng/ml on 4/14. (Any PSA value obtained after the biopsy and before the Cyberknife treatment would be invalid because of the disruption of the prostate tissue by biopsy and Cyberknife fiducal placement.) The below graphic will track the changes in my PSA value over the next 12 to 24 months.
September 2016
Week of 9/19 – The twelve week PSA post-Cyberknife value is 2.3 ng/ml. I must admit being a bit disappointed when reviewing the results. I’d expected a value in the upper 1.0+ ng/ml. Dr. C normally only evaluates 6 week and 6 month post-Cyberknife values. I elected to track the PSA score more closely. However, Dr. C indicated interest is seeing the 12 week values when they were available. I e-mailed him a copy of the total blood work document noting some disappointment in a smaller decrease in the PSA value than I’d expected. He replied that in his experienced, while the large drop in PSA immediately after conclusion of the Cyberknife therapy is normally seen – the subsequent reductions do not continue the same percentage decrease as the initial decrease. Every man is different and the lowest values may not be seen until 12-24 months post treatment. Basically, nothing to be overly concerned about.
October 2016
Week of 10/24 – The eighteen week PSA post-Cyberknife value is 1.8 ng/ml. We continue to see the slow decline of the PSA value. I’m back on my pre-Cyberknife exercise program (it was stopped when I began the Cyberknife treatment) – and like most of us, we frequently need renew our motivations to hit the gym (or in my case my home exercise equipment).
December 2016
Week of 12/05 – The twenty-four week PSA post-Cyberknife value is 1.5 ng/ml. While its impossible to predict when the PSA will break through the 1.0 ng/ml value – extending the slope of the curve would project that should occur in about 12 more weeks – assuming the current rate of decline.
January 2017
Week of 1/15 – The 30 week PSA post-Cyberknife value is 1.3 ng/ml. I’d hoped for something a bit lower – but there is sill a continued decline, only a smaller incremental drop, as compared to the values over the past 18 weeks. I was recently reviewing blood chemistry from 1999, the year my physician first began ordering PSA values for me. My PSA value from September 1999 (17 years ago) was 2.5 ng/ml. While that value from 1999 has no particular relevance to values from 2016-2017, it does provide an interesting questions – As non-cancerous prostate tissue secretes PSA, what could one define as a “cancer-free” PSA baseline values for post pubescent males? I’ll have to do some research to see if there’s any information published on that question.
March 2017
Week of 3/5 – The 38 week PSA post-Cyberknife value is 1.5 ng/ml.- not exactly what I’d expected ! A “rise” in the PSA value (when a decrease was expected) is a bit disconcerting. However, the clinical literature for Cyberknife therapy (as well as brachytherapy – radioactive pellets implanted into the prostate) documents that approximately 30% of the men receiving radiation therapies for prostate cancer will experience a PSA value “bounce”, approximately 9 to 11 months after the therapy has been completed. For me, it’s been 9 months since I completed my Cyberknife therapy. This PSA value “bounce” generally lasts between 3 to 6 months and then is followed by a continued decline in PSA values. The patients who experience the “bounce” are significantly less likely to see a reoccurrence of their prostate cancer than patients who experience no “bounce”. The cause of this PSA value “bounce” is unclear, however recent clinical publications (2016) point to some immunological response of the body to remnants of tumor cell tissue in the prostate. This response results in the transient elevation of PSA values. An e-mail to Dr. C , my radiation oncologist, returned a reply that I shouldn’t worry. While not always seen in his patients, the “bounce” is a well documented phenomena. There was no reason the suspect that Cyberknife therapy had failed.
April 2017
Week of 4/16 – The 44 week PSA post-Cyberknife value is 1.6 ng/ml – so it appears that the “bounce” isn’t over. While seeing a 0.1 ng/ml value rise from the 38 week value isn’t what was hoped for – in biological day-to-day variations over a 6 week period, the 1.6 ng/ml value means there is essentially no change from the 38 week value. So how long will the “bounce” last ? Another e-mail to Dr. C provided no answer – other than it varies from individual to individual. Nothing like a bit of suspense – but no reason to be concerned.
June 2017
Week of 6/5 – The 50 week PSA post-Cyberknife value is 1.5 ng/ml. As noted in my April entry, 0.1 ng/ml value change from the 1.6 ng/ml value of 6 weeks ago – equates to essentially no change – but it is 0.1 ng/ml LOWER rather than higher. Does this herald the end of the now infamous “bounce” ? The next PSA will be drawn during the last week in July. While I haven’t lost any sleep over the past 6 weeks about the 1.6 value, it would be nice to see something lower than 1.5 in late July.
July 2017
Week of 7/24 – The 57 week PSA post-Cyberknife value is 1.6 ng/ml. As you can see in the below graphic, we’ve basically a flat-lined value for the past 4 PSA testing points. So is this a continuation of the “bounce”, should one expect the PSA value to drop below 1.0 ng/ml, or does this indicate my response to therapy has been somewhat different than other men ? Dr. C again provided no answers – other than he’d seen patients where it took as long as 730 days (2 years) for the PSA value to drop below 1.0 ng/ml. In reviewing records of my blood chemistries and PSA values dating back 18 years, in 1999 my PSA value was 2.5 ng/ml. Certainly a graphic curve pointing to a value below 1.0 would be preferred – but, on the other hand, my PSA is almost 1.0 ng/ml lower now than in 1999 !
September 2017
Week of 9/18 – The 66 week PSA post-Cyberknife value is 1.5ng/ml. We continue to flat-lined for the past 5 PSA testing points. I’m wondering – maybe this isn’t a “bounce” after all – but rather some percentage of the prostate tissue is continuing to produce prostate tissue antigen (the measured component of the PSA test) but producing it at a “baseline level”. Because my prostate was not removed, some level of PSA would be expected even after Cyberknife therapy. Perhaps my PSA value will never fall below 1.0ng/ml – as published clinical papers would lead one to believe ? Dr. C hasn’t as yet replied to me regarding these results. I’m assuming that he’ll say a flat line is better than an upward increasing slope.
October – November 2017
Week of 10/30 – 11/3 – The 73 week PSA post-Cyberknife value remains at 1.5ng/ml, continuing the score’s flat-line values for the past 6 PSA testing points.
December 2017
Week of 12/11 – The 79 week PSA post-Cyberknife value comes in as an early Christmas gift ! FINALLY the data is showing a downward trend with this week’s value. I had met with Dr. C on the 12th, prior to the blood draw for the 79 week PSA. I think he was a bit “troubled” that the PSA value seemed to be “stuck” around 1.5ng/ml for the past 3 blood draws. The latest value of 1.2ng/ml suggest, by looking at the graph, that there has been a slow but steady decline from the “PSA bounce” of 1.8ng/ml, some 22 weeks ago.
January 2018
Week of 1/28 – The 85 week PSA post-Cyberknife value (graphic immediately below) shows a continued (but slow) decrease to 1.1ng/ml since the last blood draw 6 weeks ago. I was hoping for another 0.3ng/ml decrease from the prior reading (that would have put me under 1.0ng/ml). At least the trend is downward and not another plateau or increase. The goal is to reach 0.5ng/ml for the PSA value by (or before) the 24 month anniversary of completion of Cyberknife therapy in June 2018.
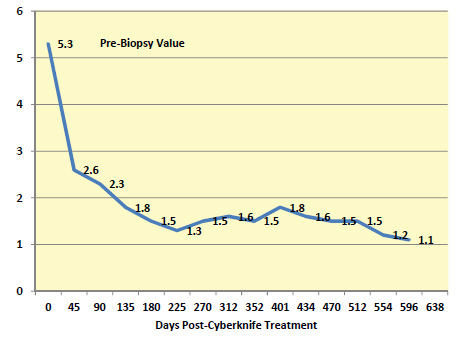
June 2018
Week of 6/10 – It’s been a hectic six month since the last post – so apologies to those who may be checking in on what historically has been an ever 6 to 7 week interval between posting.
At the end of January a friend of some 30 years died 2 days short of his 91st birthday. Being the executor of his multi-million dollar estate consumed much of my time up until recently. However, I attempted to maintain the consistent 6 to 7 week interval between PSA testing. I was well aware that one shouldn’t have a PSA test run closer than 48 hours prior to the last ejaculation. However, I found myself in a situation with a younger man the evening of 3/14, a little over 24 hours prior to my scheduled PSA test at LabCorp on 3/16. I could have cancelled the PSA test and rescheduled – but decided to go ahead with the test – day 638 on the below graphic. WOW – a PSA jump from 1.1 to 2.0 ! Well, a higher value was expected, because of the ejaculation -but the size of the increase was a bit surprising.
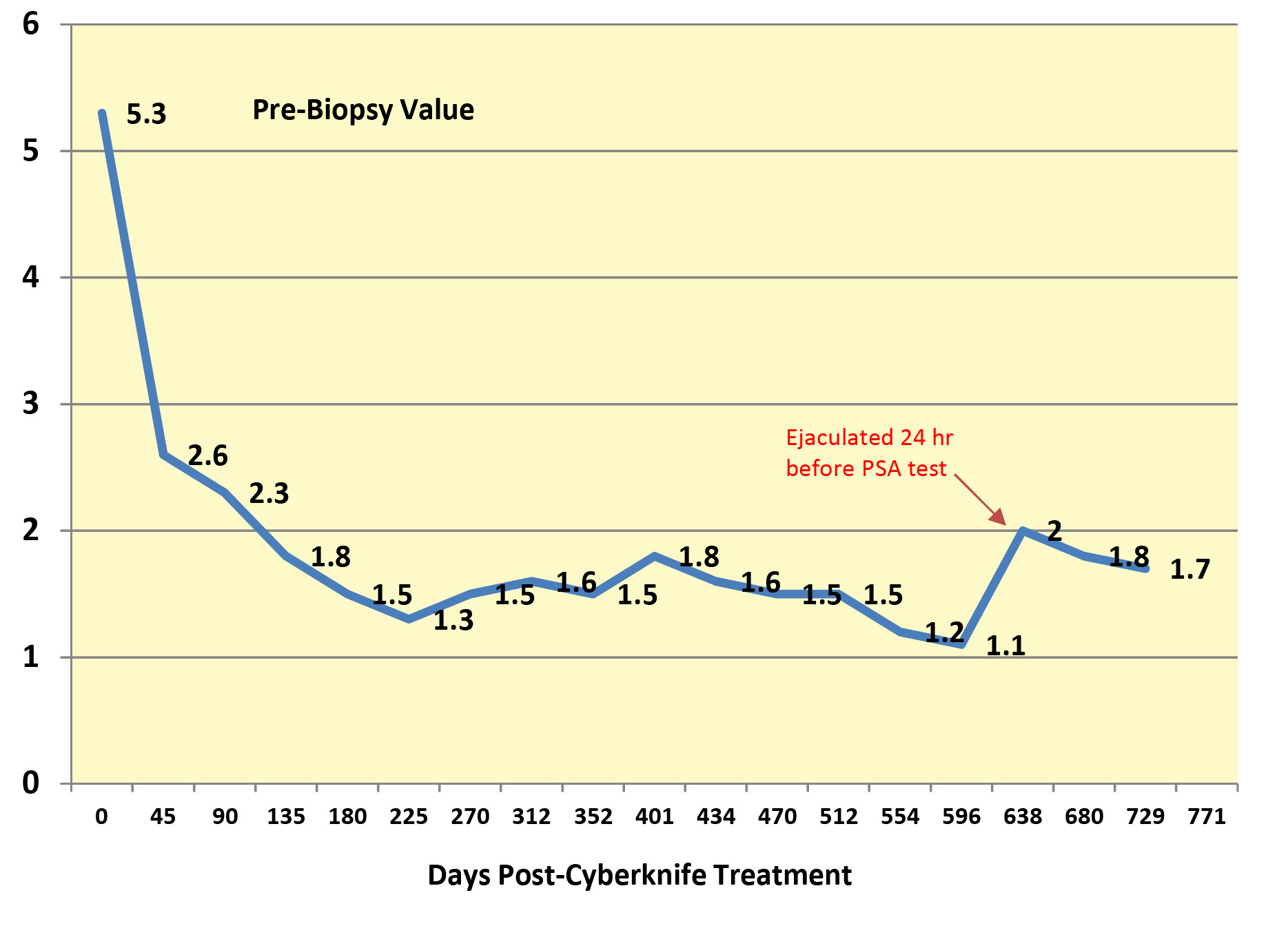
Six weeks later, day 680, because I’d been EXTRA CAREFUL to limit my sexual activity for a full week before the PSA test – I’d expected a value to be back around 1.0. But the PSA came back as 1.8. The PSA six weeks after that on day 729, the value had only dropped marginally to 1.7. Dr. C, the Cyberknife oncologist was a bit perplexed in reviewing the graphic (as was I). Clinical papers suggest that by this time, 2 years post-Cyberknife therapy, my PSA value should be below 1.0 in the 0.5 to 1.0 range. At least the values are going down !
The PSA test, the primary marker used to measure the presence of cancer in the prostate is an imperfect test – as all sorts of non-prostate factors may elevate the PSA value. Ejaculation too close to the time the test is taken, prostatitis (bacterial infection of the prostate), prostate hyperplasia (age-related enlargement of the prostate), and other sexual related activity such as anal intercourse. Being fucked by large cock may be a match made in heaven – but it’s not necessarily the best match-up if you’re tracking PSA scores.
So what’s the takeaway from all this ? (1) Don’t let your PSA value take control of your life. (2) What goes up, generally comes down – if it doesn’t – investigate WHY. (3) If you have test records stretching back a number of years – compare the current PSA value to that 5 or 10 years earlier – before you were diagnosed with prostate cancer (or had a PSA value > than 4.0. I happen to have PSA scores dating back to 2000 – 18 years ! Only once in those 18 years was my PSA value below 2.0 (in 2001, I had PSA of 1.9).
July 2018
Week of 7/01 and 7/22 – A repeat of the PSA score this week (7/01)showed a value of 1.7 and then the normal 6 week separation (7/22) between testing showed another 1.7 value. Three tests in a row at with a value of 1.7 ! Looks like some stability – even though my testosterone level (which I haven’t been discussing in this blog) went up almost 100 points in the same time period. I’m going to listen to my own advice – “Don’t let your PSA value take control of your life.” With the test of week 7/22, I’m moving the testing to quarterly (12 week cycle) rather than a 6 week cycle. The next PSA test will be the week of October 14th, 2018.
October 2018
Week of 10/14 – In early September I started taking some supplements (Boron, 9mg/day and DIMs, 150mg/day). These supplement should have an impact in enhancing testosterone production in the body as well as reducing the binding of “free” testosterone by sex hormone binding globulin (SHBG). However, higher levels of circulating testosterone and “free” testosterone might also impact the PSA value. To see if my circulating testosterone and “free” testosterone levels had gone up without impacting the PSA value – I decided to have a PSA drawn 6 weeks into the new 12 week (quarterly) cycle. The testing showed the PSA had dropped to 1.5ng/mL while my testosterone level had gone up 100 points again !
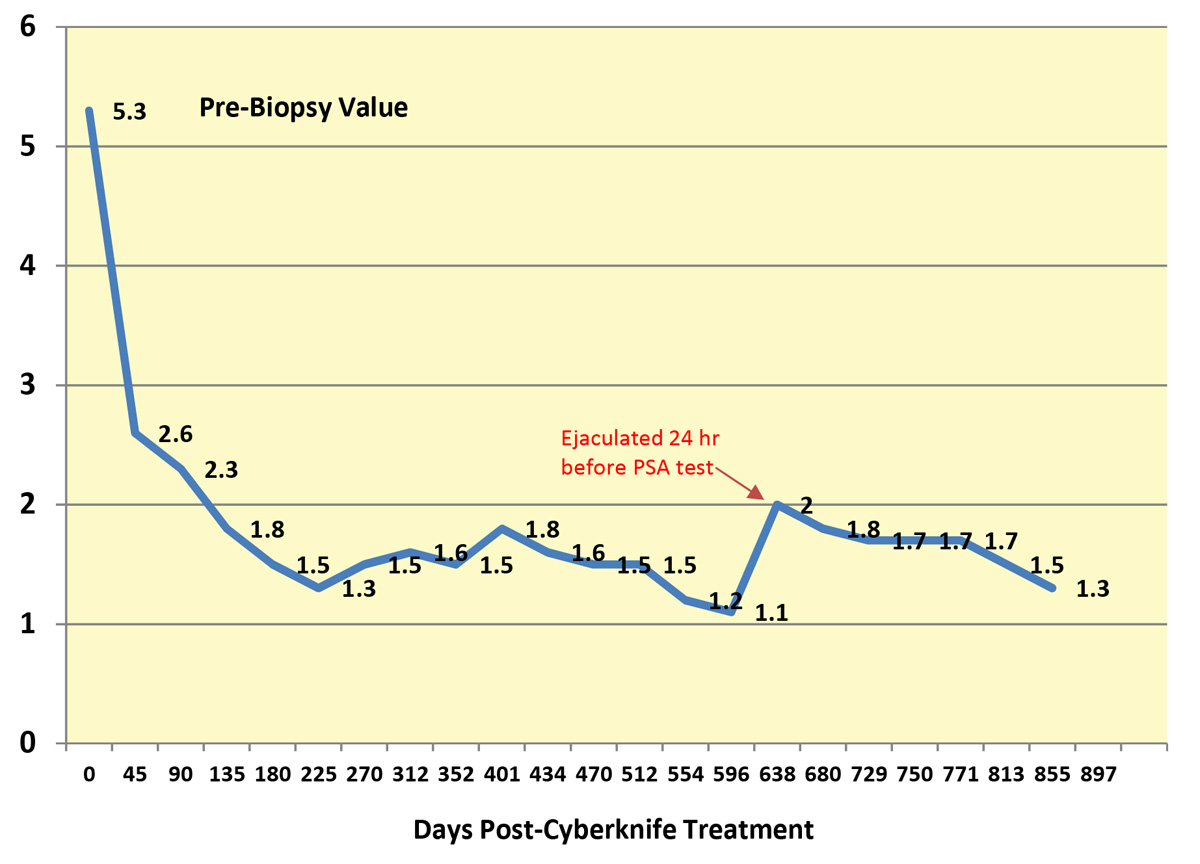
Now at approximately 855 days post Cyberknife therapy, I continue with the supplements to maintain a higher testosterone and “free” testosterone level and the PSA value has continued a slow, but steady drop. It is now at 1.3 ng/mL I’ll finish out the year with one more PSA value for 2018, probably drawn the week of December 18th.
December 2018
Week of 12/2 – With a higher testosterone and “free” testosterone levels resulting from the Boron and DIMs supplement, without any significant impact on the PSA value over the last 2 blood draws (day 813 and 855), I decided to add low level testosterone therapy to my supplement program, a few days after the blood draw of day 855. While maintaining the Boron and DIMs supplements, I added 10mg/day of a bioidentical testosterone to my supplement regimen . I use a testosterone cream (AndroForte 2) that is produced by Lawley Pharmaceuticals – http://www.lawleypharm.com.au). AndroForte, while FDA approved is not readily available in the USA. I purchase this testosterone cream from an Israeli company – http://www.testomed.com . The blood work drawn the week of 12/2 (903 days post Cyberknife therapy – see below), showed that in 7 weeks of bioidentical testosterone therapy only a 0.1ng/mL change in the PSA value was seen from day 855. My testosterone level is being maintained at about 475 ng/dL (LabCorp normal range is 264 to 916 ng/dL). I plan to continue this supplementation regimen, while monitoring the PSA value and other blood-work parameters through continued blood tests – the next blood work planned for the 1st quarter of 2019 – probably mid-March 2019.
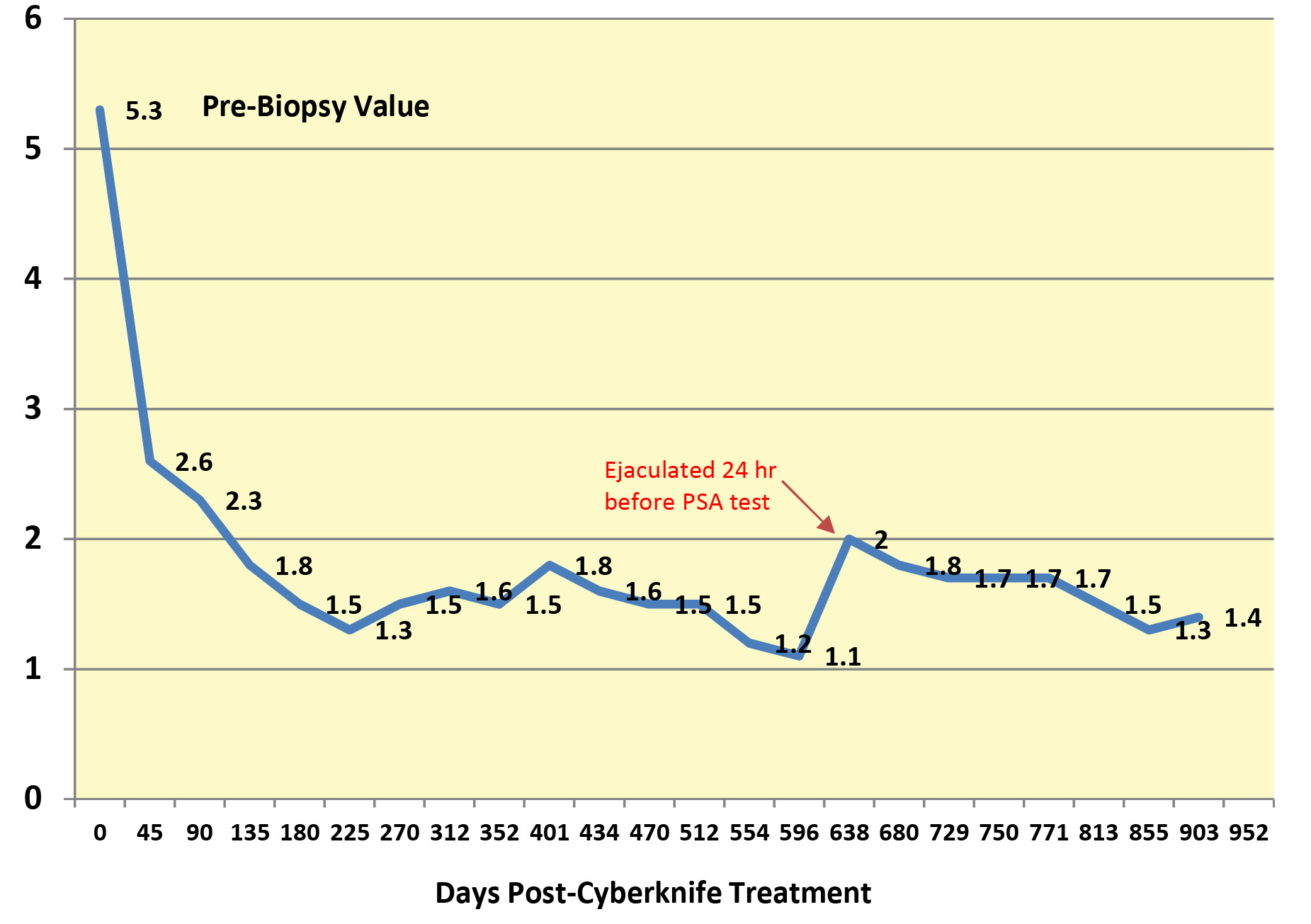
March 2019
Week of 3/24 – Since beginning bioidentical testosterone supplements in December 2018 (see week of 12/2 comments) I have continued the supplementation program over the past 90 days. The testosterone supplementation has resulted in a major impact to a renewed interest in sex and overall improvement in psychological and physiological well being. The trade-off has been a slight increase in my PSA values from 1.4 ng/ml in December 2018 to 1.8 ng/ml at the time of testing on 3/29/19 (day 1015). On meeting with Dr. C, he expressed some concern over the increase, but felt that subsequent testing would probably show a resumed PSA decrease to a level of 1.0 ng/ml (or lower).
May 2019
Week of 5/6 – A retesting to evaluate if the PSA value would continue to rise or fall, as my body adjusted to testosterone supplementation showed that on day 1050 the PSA value had dropped from the prior 1.8 ng/ml to 1.3 ng/ml. There were no changes in the level of daily testosterone supplementation.
June 2019
Week of 6/10 – This testing (day 1092) to evaluate PSA values marks 3 years since my Cyberknife treatments were completed. Both Dr. C and I were pleased to see that the PSA value for the 3 year anniversary had again moved lower from the May value of 1.3 ng/ml to 1.0 ng/ml. This strongly suggests that testosterone supplementation has not (in my case) resulting in a permanent rise in PSA values.
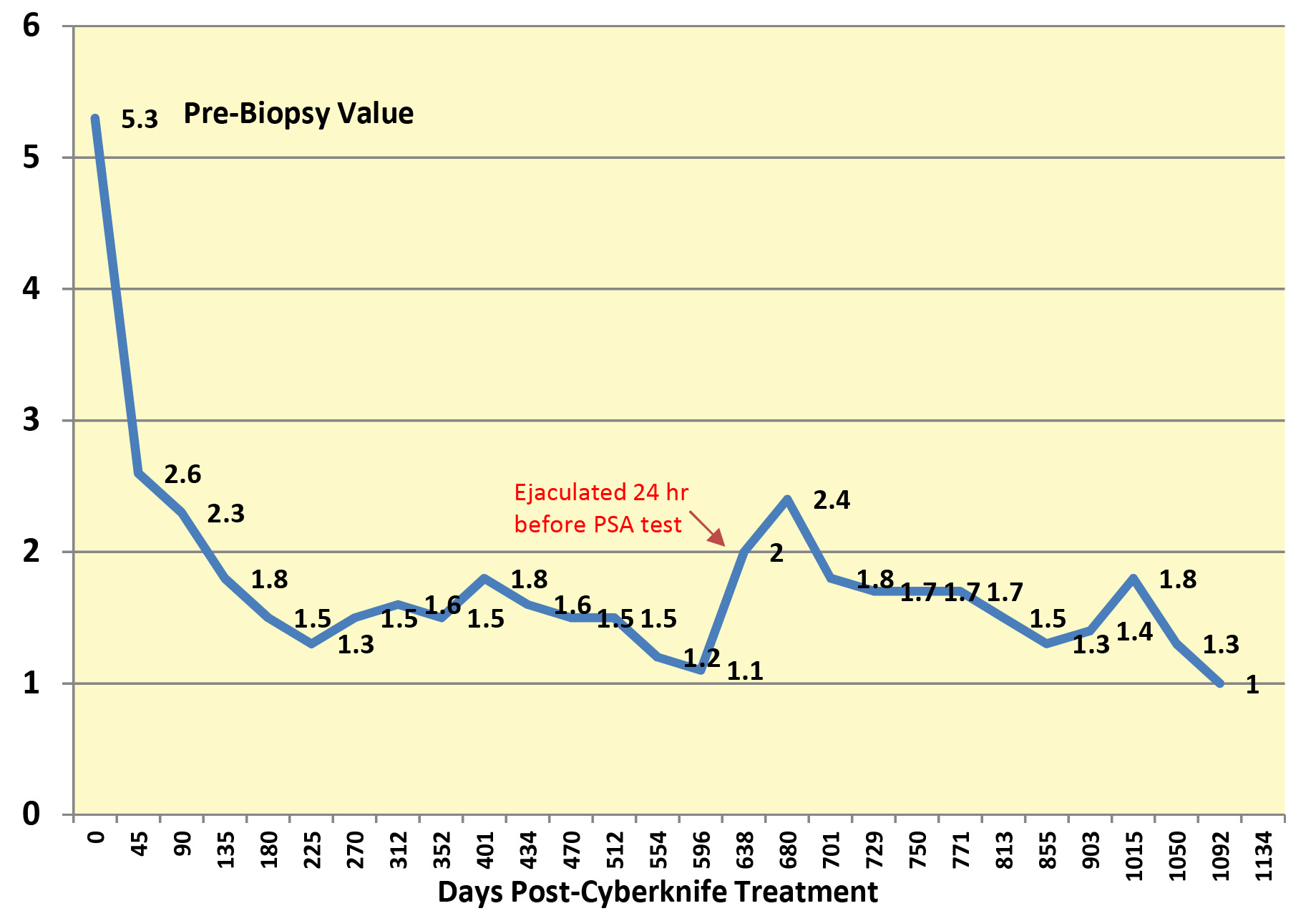
September 2019
Week of 9/23 – This testing (day 1195) to evaluate PSA values continues to confirm, by the September value of 1.1 ng/ml, testosterone supplementation has not (in my case) resulted in a rise in PSA values. The small increase of 0.1 ng/ml over the prior June 2019 value of 1.0 ng/ml falls within the probable biological variation and/or PSA test variation.
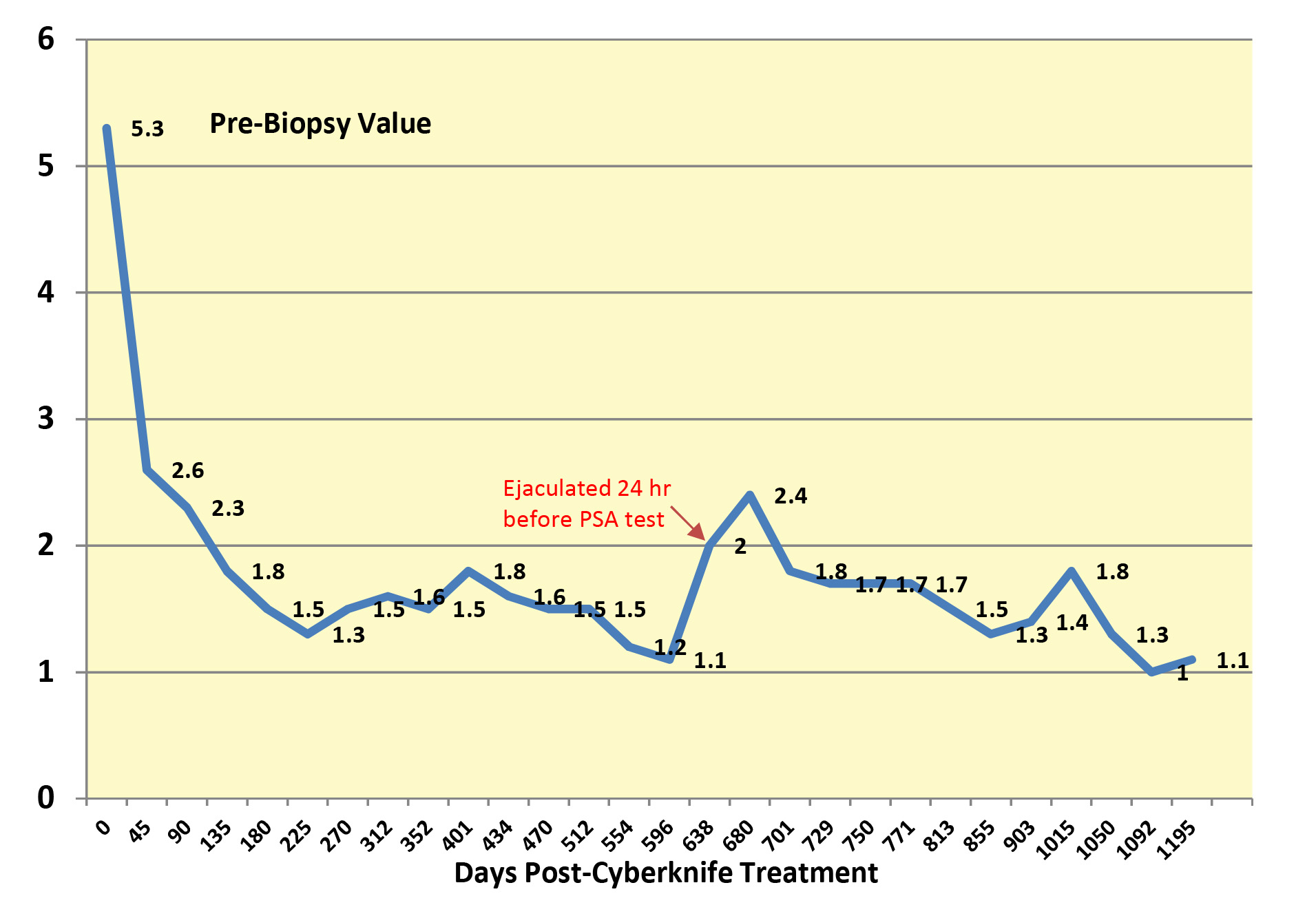
I anticipate that the next PSA testing will be done sometime during the month of December 2019.
December 2019
Week of 12/9 – This testing (day 1272) marks the first time the PSA value has fallen below 1.0 ng/ml – in this case 0.9 ng/ml. While probably not of statistical relevance (considering one would expect some biological variation in values), the PSA value are “trending” downward – which is far preferable than “trending” upward ! The value also continues to validate that in my case, testosterone supplement does not seem to be impacting PSA values.
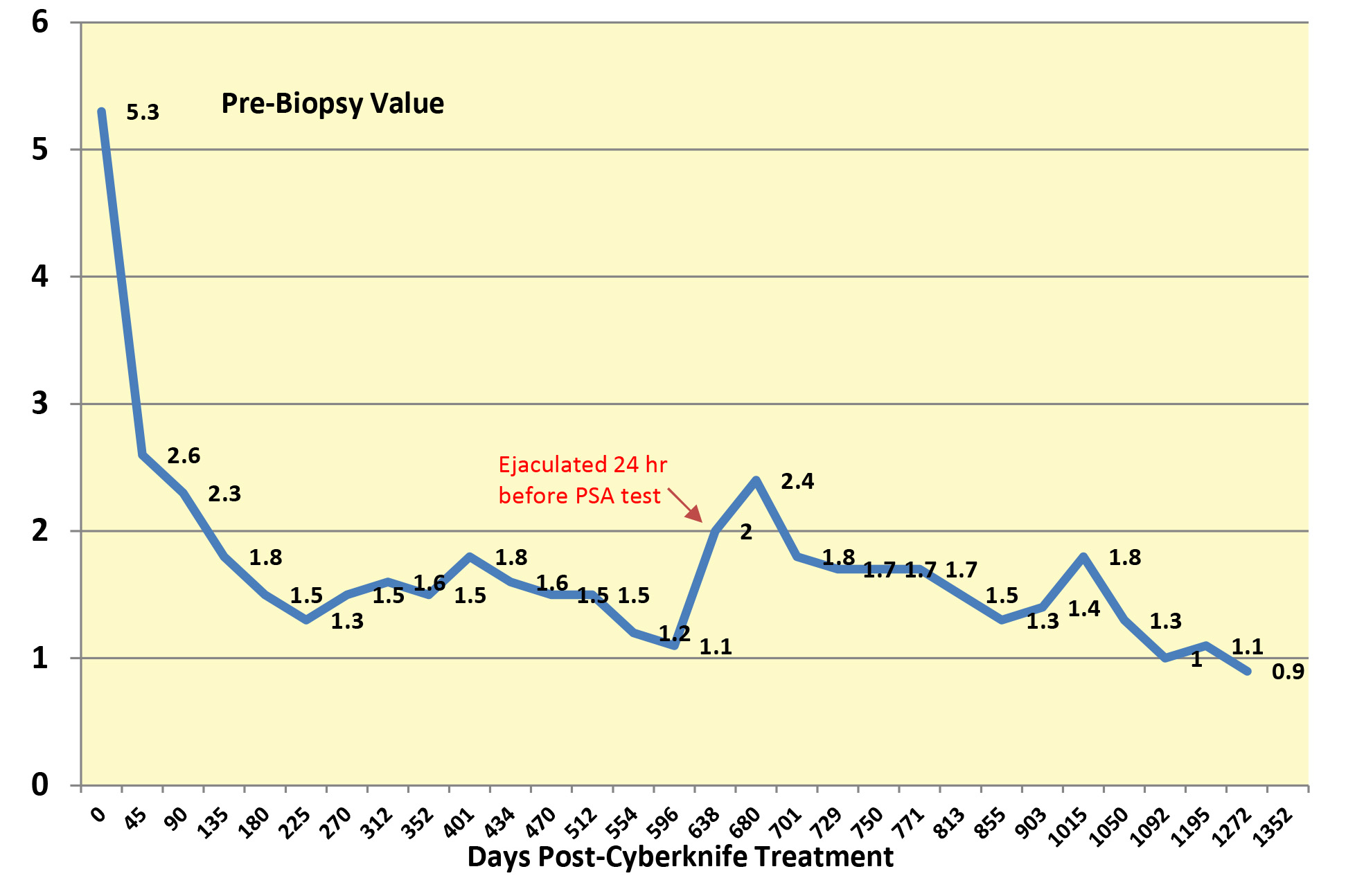
As we are now doing PSA level evaluations quarterly, I would anticipate the update on the progression of PSA values will be done during March 2020.
March 2020
Week of 3/23 – HURRAH ! This testing (day 1377) has a bit of significance in my 3.75 year post-Cyberknife therapy PSA tracking. I have have finally reached a PSA value – 0.6 ng/mL – that is very close to the magical value of 0.5 ng/mL, cited in most clinical papers as a value indicative of Cyberknife therapeutic cure. Generally this value is seen approximately 2.5 years post-Cyberknife therapy. I guess its not important as to the length of time one takes to get there – as long as one gets there !
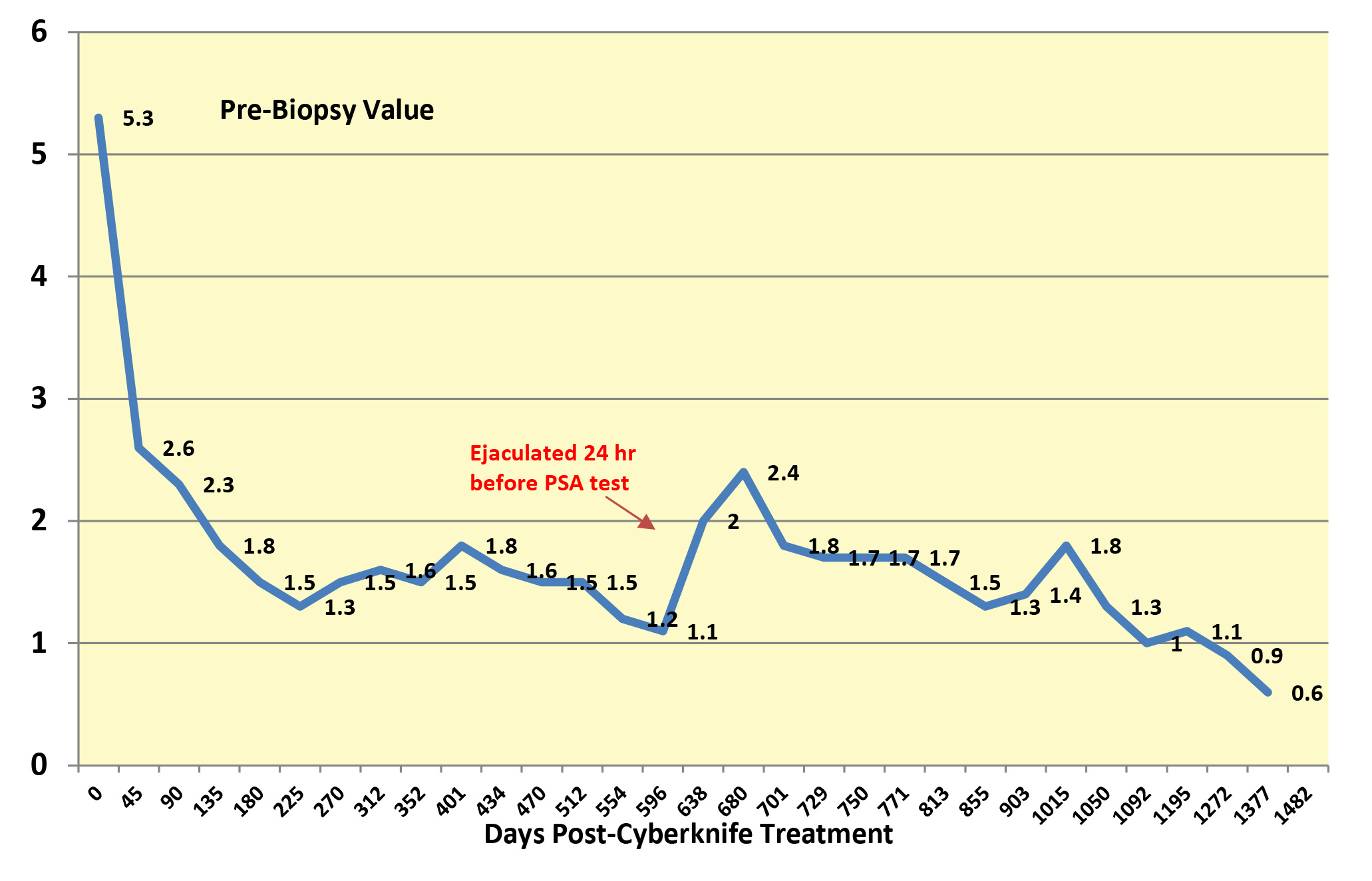
I continue to be on testosterone supplement, so the continuing decrease in PSA seems to indicated (at least in my case) that this supplement is not impacting or contributing to an elevated PSA score, when used upon completion of Cyberknife therapy.
June 2020
Week of 6/8 – This testing (day 1447) shows a slight upward “bump” from a PSA of 0.6 ng/ml to 0.9 ng/ml. Nothing to be concerned about. Probably just biological “chatter” and /or some sexual activity in the week that proceeded the blood draw. Nothing to be concerned about as the values of the last 3 PSAs have been below 1.0 ng/ml.
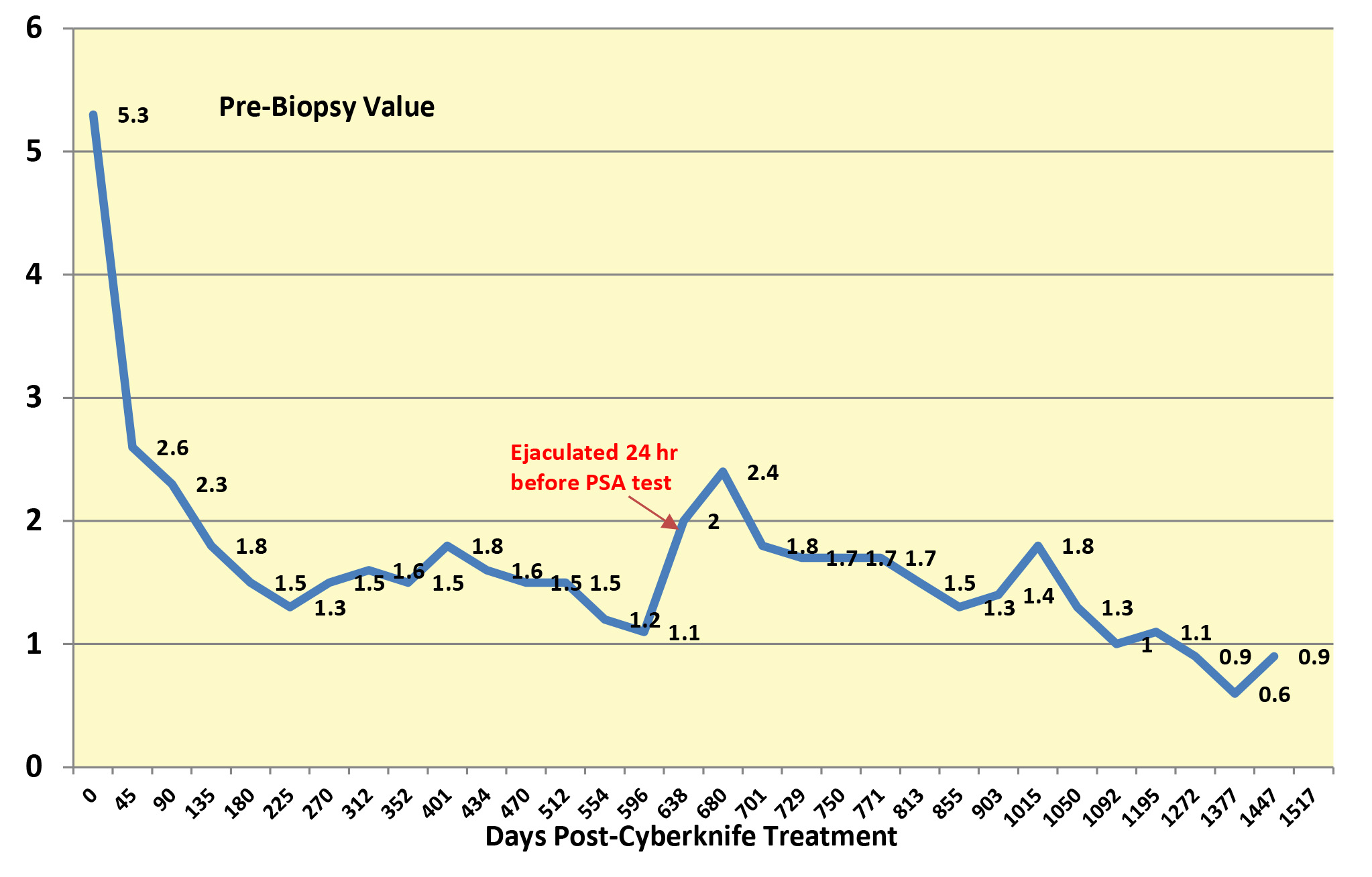
As I am now doing PSA level evaluation on a quarterly basis, it will be sometime in September 2020 for my next blood test – the 4 year anniversary of completing Cyberknife therapy!
September 2020
Week of 9/23 – This testing (day 1559) shows no change in the PSA values since the last blood draw in June – 0.9ng/ml. The next PSA evaluation will be in December 2020.

January 2021
Week of 1/13 – This testing (day 1671) shows a small decrease in the PSA value (0.7ng/ml) since the last PSA value of September 2020, (0.9ng/ml). I did not have any blood work done in December 2020 as both of my urology/ radiation oncology physicians postponed an office visit due to the COVID-19 pandemic. The past 3 PSA values have all been below 1.0ng/ml and exhibit the biological up/down bottoming values associated with treatment where the prostate (organ) has not been removed by surgery.

July 2021
Week of 7/13 – This testing (day 1798) shows a small increase (0.1ng/ml) in the PSA value, since the last PSA value of January 2021. The past 4 PSA values have all been below 1.0ng/ml. The July 2021 PSA value is 0.8ng/ml. The up/down variation of PSA values continue to show that while the values have not continued to trend downward – they have stabilized in a range between 1.0 and 0.5 ng/ml. The up/down variation reflects biological variation as well as possible test procedure variations.

It’s now been 5 years since my completion of Cyberknife therapy for prostate cancer. With the July 2021 PSA testing, as my PSA values are stable, I have decided to make this the last posted entry in my blog. While I may not be a text book “poster child” for a radiation oncologist, I feel my decision to use Cyberknife was the correct one. Unlike men who elect to have surgery for prostate cancer – I have not experienced any urinary problems (incontinence) or sexual impotency issues that could be related to Cyberknife therapy. There was no protracted recovery down-time for this treatment. Life has continued on with its normal mix of surprises and disappointment, as before the diagnosis of prostate cancer.
For those who have taken time to peruse this blog over the past 5 years, I hope that my experience with prostate cancer and Cyberknife therapy has been useful to help you (if impacted by a diagnosis of prostate cancer) form your own decision about how to resolve this life changing event.
While each man’s unique biopsy’s Gleason Score will be the best indicator of which of the multiple of technologies currently available may be the one to optimally treat his prostate cancer and minimize its metastasis – one should always explore one’s options before making a decision. That decision will be a largely irreversible one and will impact the balance of ones life.

Thanks for the detailed reports. I am going through my process. I had my gold seeds placed and getting ready for my MRI and CT scan. I had to argue with an Anesthesiologist as I did not want intubated and he was insisting until I reminded him of the Patient’s bill of rights. My Urologist supported my decision and I did agree to conscious sedation for the procedure. Seems the full process is taking allot longer than I anticipated.
Ross B. Tulsa, OK
LikeLike
I think the most difficult part of the entire Cyberknife experience, for prostate cancer therapy, was the placement of the fiducials (gold seeds) and (in my case) the placement of the SpaceOAR materials to minimize radiation damage to the rectal intestine. General anesthesia was never considered – I used local as it allowed me to not need someone to drive me home after the procedure. Your note suggests that you selected some type of radiation therapy (Cyberknife?) – I hope that your treatments will result in a favorable outcome of your diagnosis.
LikeLike
Cyberknife is the treatment I am headed for. That is why I had to argue with the Anesthesiologist about General Anesthesia for the placement of the fiducials and the spacer gel. They don’t seem to be knowledgeable in Tulsa as to how this is done. I was the first patient here to receive a new type of gold fiducial seeds they are starting to use here.
LikeLike
Ross B – It appears from a web search there are 2 Cyberknife facilities in Tulsa. It’s good to know that you have received the SpaceOR gel. That suggests that the radiation oncology team is utilizing the most recent technology to minimize radiation damage to intestinal tissue adjacent to the prostate. Good luck with your Cyberknife sessions !
LikeLike
You are absolutely amazing with your attention to detail and all of the research and investigating you have done. I so appreciate your blog and look forward to talking with you in the future and see if this might be the route I take
LikeLike
Thanks for your kind comment on the blog. I think that the decision on which of the many treatment options available should be based upon one’s biopsy report’s Gleason Scores and if the cancer is confined to the prostate. Remember most urologists will recommend surgery over any type of radiation therapy – follow the money – urologists whose specialty is prostate cancer are probably surgeons too. If you do elect surgery, make sure that the urology surgeon used a nerve conduction monitor (PROPEP Surgical) during the robotic surgery. Nerve conduction monitoring can minimize the side effects of urinary incontinence and sexual dysfunction. Cyberknife therapy minimizes these two side effects and essentially zero recovery time after treatment.
LikeLike
I am a 68 year old man recently diagnosed in November. Been with my husband for thirty years. We both still enjoy an active sex life with each other and looked into what would be the best option for us. Thanks for the detailed blog of your journey. I have also elected to have cyberknife for my prostate cancer. Simular numbers to yours. This Wednesday March 4th 2020 I will have my gold markers and spaceoar gel put in. Feeling a bit anxious about not being put under and the thought of the needles. Wishing you continued good PSA scores and good health.
LikeLike
Have you ever thought about publishing an ebook or guest authoring
on other sites? I have a blog based upon on the same topics you discuss
and would love to have you share some stories/information. I know my readers
would enjoy your work. If you are even remotely interested, feel free to shoot me an e-mail.
LikeLike
Thank you for taking time to drop me a comment about my blog site. The site was created back in 2016 to provide a way for me to record an opportunity that generally only comes once in one’s life – a life-threatening condition. Because of my educational and professional background, it seemed like the natural thing to do. I’ve never given any thought to publishing an ebook – but do have an ongoing interest exploring the role of minerals – lithium, zinc and magnesium in maintaining good mental and physical health. I would be happy to communicate more with you (as long as there would be little or no financial commitments from me, in what you might have in mind).
LikeLike